Opioids over-prescribed after hiatal hernia surgery
The increase in opioid deaths in the last 20 years led a medical student at the University of Michigan Medical School and colleagues to look at excessive opioids prescribed to treat acute surgical pain following various procedures. Alyssa A. Mazurek presented a study during the American Association for Thoracic Surgery's 98th Annual Meeting that assessed patterns of opioid prescribing for open and laparoscopic hiatal hernia repair (HHR) and found that patients used far fewer opioids than were actually prescribed.
"The deadliness of the opioid epidemic has become one of the largest public health crises of our time, and its devastating effects are felt throughout the country," explains Mazurek, who presented the study results during a moderated poster session. "However, there has been very little investigation into opioid prescribing practices after thoracic surgeries. Further investigation is needed to understand what mechanisms are contributing to excessive prescribing and morbidity, such as opioid dependence, addiction, and narcotic diversion, associated with postoperative opioid use."
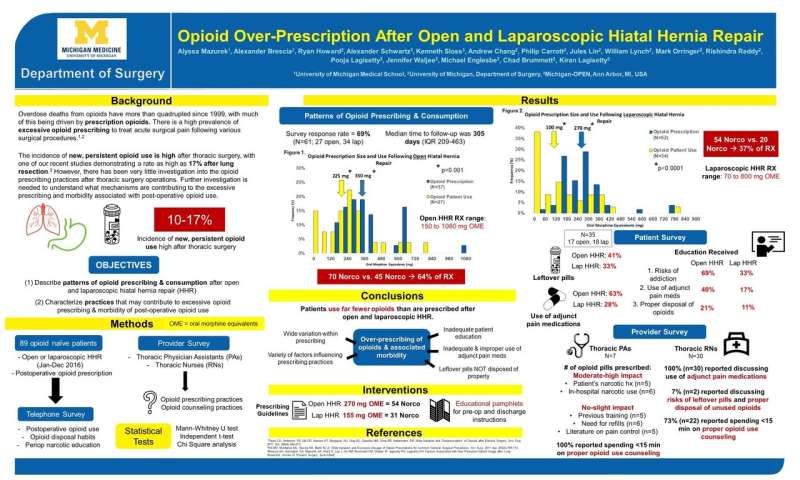
Investigators reviewed the charts of 89 "opioid naïve" patients who underwent open (including transthoracic and transabdominal) or laparoscopic HHR between January and December 2016, and who had received an opioid prescription after surgery. "Opioid naïve" was defined as patients not taking an opioid at the time of their preoperative history and physical. Their objective was to describe the patterns of opioid prescribing and consumption after open and laparoscopic hiatal hernia repair (HHR); and to characterize the practices that may contribute to excessive opioid prescribing and morbidity of postoperative opioid use.
Patients were surveyed regarding postoperative opioid use, opioid disposal habits, and any narcotic education received. Sixty-nine percent of patients completed the survey, of whom 27 had open surgery and 34 had laparoscopic surgery. Thoracic physician assistants and nurses (RNs) were surveyed regarding factors that contribute to their opioid prescribing and counseling practices.
The results showed that patients used far fewer opioids than were prescribed after both open and laparoscopic HHR. Patients only used 52 percent of narcotics prescribed to them, with a significant number of patients reporting leftover pills due to lack of proper disposal, a combination that provides a dangerous source for narcotic diversion. The investigators identified several factors that may be contributing to over-prescribing of opioids and the associated morbidity of postoperative opioid use, including: wide variation within prescribing; variety of factors influencing prescribing practices that differ among providers; inadequate patient education; inadequate and improper use of adjunct pain medications; and leftover pills not disposed of properly.
"It has become clear that surgeons and other healthcare providers play a major role in the over-prescribing of opioids after surgery," says Mazurek. Various studies have demonstrated the high prevalence of and detrimental long-term consequences of continuing to use opioids after surgery, such as opioid dependence/addiction, opioid overdose, and narcotic diversion.
Mazurek concludes that, "Given the growing awareness of this epidemic and the willingness of surgeons around the country to address it means we can also play a huge role in reducing excessive opioid prescribing and the number of unused pills that permeate into the community by further understanding prescribing practices and creating procedure-specific guidelines."
More information: "Opioid Over-Prescription After Open and Laparoscopic Hiatal Hernia Repair," by Alyssa A. Mazurek, Alexander Brescia, Ryan Howard, Alexander Schwartz, Kenneth Sloss, Andrew Chang, Philip Carrott, Jules Lin, William Lynch, Mark Orringer, Rishindra Reddy, Pooja Lagisetty, Jennifer Waljee, Michael Englesbe, Chad Brummett, and Kiran Lagisetty. Presented by Alyssa A. Mazurek at the AATS 98th Annual Meeting, April 28-May 1, 2018, San Diego, Calif., at the Moderated Poster Session on Tuesday, May 1, 2018. The abstract for this presentation can be found at: aats.org/aatsimis/AATS/Meeting … m/Abstracts/P30.aspx
















