New lab technology could reveal treatments for muscle-wasting disease
Researchers from Queen Mary University of London have developed new cell-based technologies which could help improve understanding of the muscle-wasting disease Duchenne muscular dystrophy (DMD) and test potential drugs for the disease.
DMD is a genetic disorder causing muscle degeneration and weakness, caused by an absence of the protein dystrophin. DMD usually affects only boys, with around 100 being born with the condition in the UK each year. There are about 2,500 males known to be living with the condition in the UK at any one time.
There are currently no effective treatments for the disease, and patients often succumb to cardiomyopathy, a weakness of the heart muscle which can be fatal. Significant advances have been made in treating DMD in animal models, but there has not yet been success in translating this into medicines for DMD patients.
The new approach, led by Dr. Yung-Yao Lin from Queen Mary's Blizard Institute and supported by Professor Andy Tinker from Queen Mary's William Harvey Research Institute, uses the latest advances in gene editing and stem cell technology to develop a model of human cells with DMD which mimic what happens in a patient's muscles.
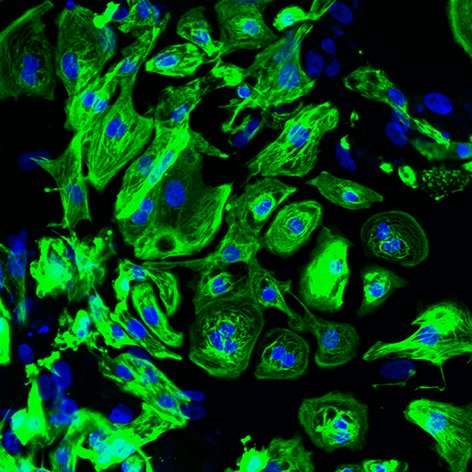
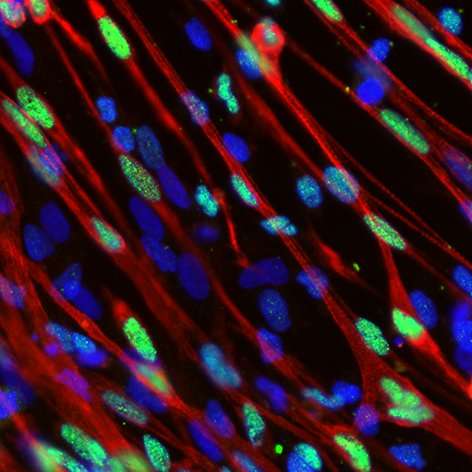
The team will be using 'induced pluripotent stem cells'—adult cells which have been reprogrammed to an embryonic state, so that they can grow to become any type of cell in the body—in this case, skeletal and cardiac muscle cells.
A challenge with comparing diseased and healthy cells in research, however, is that each donor's muscle cells have a different genetic make-up. This makes it incredibly difficult to accurately demonstrate functional differences between DMD patient and healthy human donor muscle cells.
To overcome this, the researchers have made use of a gene editing tool known as CRISPR. CRISPR is in use by medical researchers all over the world, but normally it is only used to delete sections of DNA—a relatively simple process.
Here, the team are using CRISPR to instead carry out precise editing of the genetic code within DMD patients' stem cells to 'fix' the code and create a healthy muscle cell which has the same genetic make-up as the original patient's cell.
Dr. Yung-Yao Lin from Queen Mary's Blizard Institute said: "Dystrophin is the largest gene in humans, comprising 2.4 million base-pairs and 79 separate protein-coding regions. This makes it one of the most difficult genes to correct, but we've managed to do it.
"We can now use DMD patient skin cells which are stored in the biobank, and turn them into stem cells to generate an unlimited supply of skeletal and cardiac muscle cells in culture dishes. Our genetically-corrected stem cells will also help us establish a cell-based platform to test future drug candidates."
Mark Silverman from the board of trustees of Action Duchenne, a charity supporting muscular dystrophy research, said: "As both a parent and member of the research committee at Action Duchenne, it is very encouraging to see the breakthrough CRISPR editing tool being used in this way.
"There remains a large, unmet need for treatments in Duchenne and families affected by this devastating condition want to see more rapid testing of potential treatments. This exciting news coincides with the release of our latest research strategy, which builds on Action Duchenne's experience in identifying innovative state-of-the art research."
Professor Francesco Muntoni from the MRC Centre for Neuromuscular Diseases said: "We established a rare diseases biological samples biobank to facilitate research on pathogenesis and translational research for children and adults affected by neuromuscular disorders. I am pleased to see this invaluable resource has played a key role in addressing unresolved questions of pathogenesis of Duchenne muscular dystrophy and is being used to develop novel therapeutic strategies."
The research project to further develop these cell-based technologies for DMD stemmed from the Rare Disease Consortium Initiative, a five year agreement between Pfizer and the Global Medical Excellence Cluster, of which Queen Mary is one of several university partners. The Rare Disease Consortium Initiative provides resources and a framework for the research and development of new and innovative medicines for rare diseases.


















