In MS, disintegrating brain lesions may indicate the disease is getting worse
For decades, clinicians treating multiple sclerosis (MS) have interpreted the appearance of new or expanding brain lesions on magnetic resonance imaging (MRI) scans as a sign that a patient's disease is getting worse. Now, University at Buffalo researchers are finding that it may be the atrophy or disappearance of these lesions into cerebrospinal fluid (CSF) that is a better indicator of who will develop disability.
The five-year study, conducted by MS researchers in the Jacobs School of Medicine and Biomedical Sciences at UB, was published in the Journal of Neuroimaging. Similar findings also resulted from their 10-year study of 176 patients that they presented at the annual meeting of the American Academy of Neurology (AAN) in Los Angeles in April.
Robert Zivadinov, MD, PhD, first author on the 10-year study and senior author on the five-year study, said: "Using the appearance of new brain lesions and the enlargement of existing ones as the indicator of disease progression, there was no sign of who would develop disability during five or 10 years of follow-up, but when we used the amount of brain lesion volume that had atrophied, we could predict within the first six months who would develop disability progression over long-term follow-up."
Zivadinov, a professor of neurology in the Jacobs School and director of the Buffalo Neuroimaging Analysis Center (BNAC) in the Jacobs School, also directs the Center for Biomedical Imaging at UB's Clinical and Translational Science Institute.
Brain lesions and MS
Brain lesions in general are a sign of damage to the brain, such as physical trauma, a stroke, normal aging or chronic disease. Patients with MS receive MRI scans as part of their routine care so that doctors can track the appearance of new lesions and the enlargement of existing ones, typically seen as indicators of disease progression. Approval by the Food and Drug Administration for new MS drugs typically depends on the drug's ability to reduce the number of brain lesions over 24 months.
Zivadinov noted that according to this premise, the loss of brain lesions could inadvertently be seen as a sign that the patient's condition is improving. MS is characterized by the loss of myelin sheaths surrounding axons in the brain and disrupting the brain's ability to send and receive neuronal messages. The growth of new myelin sheaths around axons may demonstrate that some brain tissue has been repaired spontaneously or as the result of medication.
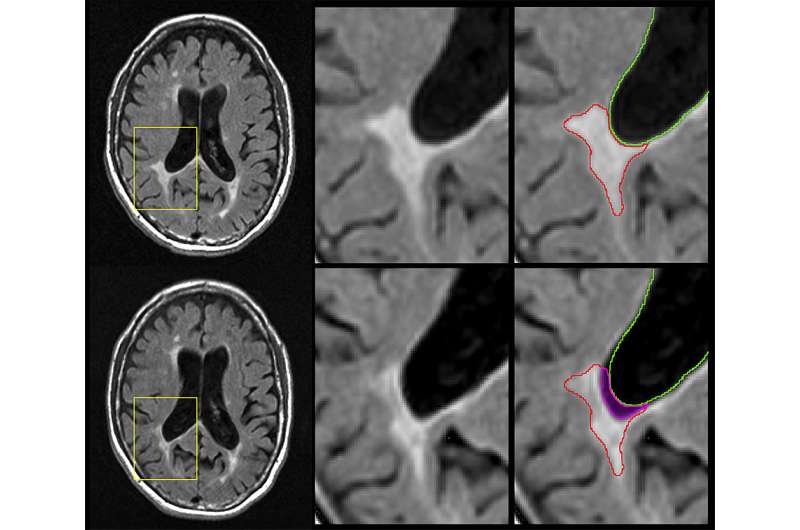
In order to focus specifically on the disappearance of lesions that likely indicate pathological change like atrophy, not beneficial change, like resolution or remyelination, the researchers looked exclusively at lesions seen on previous scans that were later replaced by cerebrospinal fluid.
"How do we know the lesions have disappeared?" asked Zivadinov. "Because where there was brain lesion tissue before, there now is just fluid."
Lesions disappearing into cerebrospinal fluid
"The big news here is that we did the opposite of what has been done in the last 40 years," said Michael G. Dwyer, PhD, assistant professor of neurology and bioinformatics in the Jacobs School and first author on the five-year study in the Journal of Neuroimaging. "Instead of looking at new brain lesions, we looked at the phenomenon of brain lesions disappearing into the cerebrospinal fluid."
The researchers looked specifically at the rate of brain lesion loss due to atrophy compared to accumulation of lesion volume seen both at baseline and follow-up. They found that the amount of lesion volume that atrophied was the only significant lesion parameter that correlated with clinical disability as measured by the Expanded Disability Status Scale (EDSS), the most widely used method of quantifying disability in MS.
"We didn't find a correlation between people who developed more or larger lesions and developed increased disability," said Dwyer, "but we did find that atrophy of lesion volume predicted the development of more physical disability."
While patients with relapsing remitting MS showed the highest amount of new lesions during the study, patients with progressive MS—the most severe subtype—had the most accelerated volume of brain lesion atrophy. The UB researchers said this indicates that this new imaging biomarker could be particularly important in transitional phases between relapsing and progressive MS subtypes.
"Paradoxically, we see that lesion volume goes up in the initial phases of the disease and then plateaus in the later stages," said Zivadinov. "When the lesions decrease over time, it's not because the patient lesions are healing but because many of these lesions are disappearing, turning into cerebrospinal fluid."
More robust than whole brain atrophy
Another important scientific finding of the studies, Zivadinov continued, is that atrophied brain lesions were a more robust predictor of disability progression than the development of whole brain atrophy itself, the most accepted biomarker of neurodegeneration in MS.
"Our data suggest that atrophied lesions are not a small, secondary phenomenon in MS, and instead indicate that they may play an increasingly important role in predicting who will develop a more severe and progressive disease," he said.
The five-year study involved 192 patients with one of the three subtypes of the disease: clinically isolated syndrome, the earliest stage; relapsing remitting, an intermediate stage; or progressive, the most severe stage. In that study, patients underwent imaging studies in the Center for Biomedical Imaging in the Clinical and Translational Science Institute at UB and BNAC.
The volume of lesions was quantified at the start of the study and patients received yearly scans on the same 3 Tesla MRI machine for more than five years. Lesion volumes were calculated over the five years of the study.
More information: Michael G. Dwyer et al. Atrophied Brain Lesion Volume: A New Imaging Biomarker in Multiple Sclerosis, Journal of Neuroimaging (2018). DOI: 10.1111/jon.12527

















