Breaking the link between obesity, gastrointestinal cancers
Studies have demonstrated a connection between obesity and a person's risk of developing colon and other gastrointestinal cancers. Now, scientists are investigating approaches that can break this relationship.
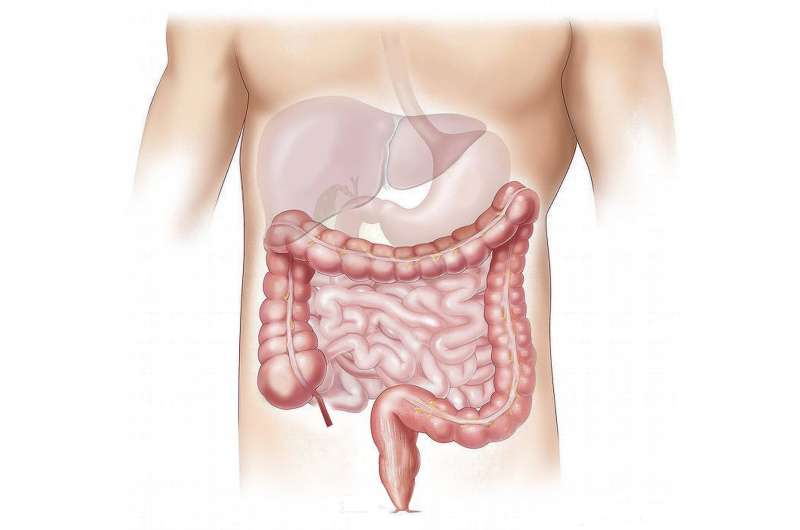
In an article in the journal Nature Reviews Gastroenterology & Hepatology, UNC Lineberger's Stephen Hursting, Ph.D., MPH, along with Cornelia Ulrich, Ph.D., MS, the director of the Huntsman Cancer Institute's National Cancer Institute-designated Comprehensive Cancer Center, and colleagues, reviewed findings from research looking at the biological links between obesity and cancers of the colon, rectum, pancreas, liver, esophagus, gallbladder and stomach, as well as published studies on how diet, exercise, weight loss surgery, and other weight-related interventions may help reverse this connection.
Obesity has been linked to 13 different cancers, including several cancers of the gastrointestinal system, making it the "second leading cause of cancer after smoking," according to an expert panel convened in 2016 by the International Agency for Research on Cancer that included Ulrich and Hursting.
"Obesity has emerged as a major risk factor for several gastrointestinal cancers," said Hursting, who is a professor of nutrition at the UNC Gillings School of Global Public Health and the UNC Nutrition Research Institute. "There are lessons from studies of these cancers that are suggesting possible ways to reverse the effect of obesity on cancer risk."
Hursting and his collaborators reviewed findings from a number of clinical trials that examined the effects of diet and other interventions on the prevention of gastrointestinal cancers, and the impact of physical activity, diet and weight loss surgery on mortality and other outcomes after a person has been diagnosed.
One study, the Women's Health Initiative Dietary Modification trial, investigated the effect of lowering fat intake while increasing consumption of grains, vegetables and fruits in preventing cancer in 48,835 postmenopausal women. The researchers reported the dietary changes did not reduce long-term colorectal cancer risk, but it did lead to reduced incidence of pancreatic cancer among overweight or obese women.
They also reviewed studies of bariatric surgery, a surgical weight loss intervention that often results in rapid body weight reduction and changes in biological markers of cancer risk in extremely obese individuals. Hursting and his colleagues wrote that the results of observational studies of cancer incidence after bariatric surgery suggest that weight loss surgery is associated with lower incidence of several obesity-linked gastrointestinal cancers, including esophagus, pancreas and liver cancer.
"The data is emerging that in the face of chronic obesity, a rapid, sustained metabolic change as achieved with bariatric surgery seems to reverse many pro-cancer effects of obesity," Hursting said. "A current focus of my laboratory is to understand the mechanisms involved in the anti-cancer effects of bariatric surgery and to identify combinations of dietary, exercise or pharmacologic interventions that can mimic the benefits of bariatric surgery without having to go through the surgery."
The authors' review of studies of interventions after a cancer diagnosis revealed that calorie restriction and exercise have "demonstrated benefits both during and after treatment" for patients who have cancers of the gastrointestinal system. While there have been no randomized controlled trials, epidemiological evidence from studies at the population level have shown that physical activity among survivors reduces the risk of death from colorectal cancer by almost half.
"Some of the clearest data from both animals and humans regarding the reversibility of the pro-cancer effects of obesity come from studies of colon cancer," Hursting said.
Lastly, they examined how weight loss, physical activity, diet exercise and bariatric surgery impact biological mechanisms that are linked to cancer, such as inflammation.
"We've tried to assess the mechanistic pathways that underlie the obesity-gastrointestinal cancer link," Hursting said. "There are some well-established mechanisms, including systemic inflammation, adipose tissue changes, and signals from obesity-associated growth factors, such as insulin and insulin-like growth factors. Within the colon, there is a lot of interest in the role of the microbiome as well, and how colonic bacteria may be interacting with obesity to effect the tumor microenvironment.
More information: Cornelia M. Ulrich et al. Energy balance and gastrointestinal cancer: risk, interventions, outcomes and mechanisms, Nature Reviews Gastroenterology & Hepatology (2018). DOI: 10.1038/s41575-018-0053-2




















