To resolve inflammation, location matters
Health conditions that involve inflammation run the gamut, from multiple sclerosis and lupus to arthritis, diabetes, and cancer. While inflammation can serve as a normal response to help the body deal with injury or infection, problems arise when it persists, potentially harming surrounding tissues.
To prevent or ameliorate this damage, the body relies on a strategy to actively clear inflammation. "It's not just extinguishing the fire of inflammation," says George Hajishengallis of the University of Pennsylvania. "You also have to return things to the way they were before the inflammatory destruction."
A new study led by Hajishengallis, the Thomas W. Evans Centennial Professor in Penn's School of Dental Medicine, and Triantafyllos Chavakis of the Technical University of Dresden has illuminated a key player in this resolution process, the protein Del-1, which the pair has studied extensively before. While prior research had underscored Del-1's role in curbing the initiation of inflammation, the new work finds that it can serve a very different function, actively working to clear inflammation. Which function the protein performs depends on the cell type that expresses it, the team found.
"Our findings prompted us to propose the 'location principle' in the spatial regulation of the immune response," says Chavakis. "In other words, homeostatic molecules—those responsible for maintaining equilibrium in the body—may perform different regulatory functions depending on their location."
The work appears in the journal Nature Immunology.
Hajishengallis, Chavakis, and their labs and collaborators have been interested in the protein Del-1 for many years. Through a series of experiments and publications, they've established its importance in the initiation of inflammation. Focusing on periodontitis, severe gum disease, as a model system, they've found Del-1 restrains the activity of neutrophils, preventing damaging inflammation and bone loss in the gums.
In the new work, they wanted to see whether Del-1 could also act not just to hold back inflammation from occurring in the first place but also to actively resolve it once it occurred.
In collaboration with co-author Jonathan M. Korostoff, professor of periodontics at Penn Dental Medicine, they found that, in humans with periodontitis, Del-1 levels rose upon treating the disease. To follow up on the finding and get at a mechanism, they turned to a mouse model of gum disease, observing that Del-1 expression levels rose when the animals' disease began to resolve, a mirror to the human data.
"Just because Del-1 goes up doesn't necessarily mean anything," says Hajishengallis, "but, when we did the same experiment with mice that lack Del-1, the resolution of inflammation failed."
That suggested to the scientists that Del-1 was a necessary component of the resolution process. To further explore this possibility, they turned to another disease, peritonitis, which involves inflammation of the abdominal lining.
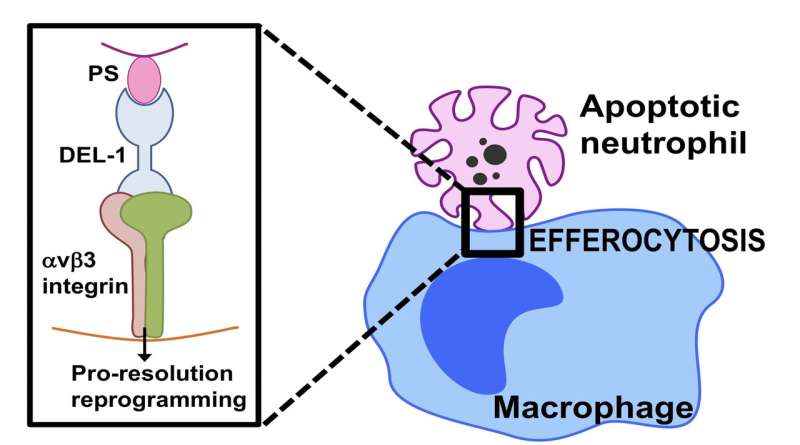
Here they saw the same effect and were further able to show a course of action: Del-1 was able to act as a molecular bridge to expedite the clearance of dying neutrophils by connecting them to macrophages, a distinct type of immune cells that engulf and "eat" cellular debris, and thus maintaining a healthier environment. This process of clearing dying neutrophils is called efferocytosis.
Importantly, Del-1 appeared to reprogram the efferocytic macrophages toward a type that contributes to resolution and tissue repair. Mice lacking a domain of Del-1 that interacts with macrophages were not able to promote efferocytosis.
In addition to promoting this clearance of neutrophils, the researchers discovered that Del-1 also induced a group of molecular mediators called resolvins, which promote inflammation resolution. The researchers hypothesize that Del-1 may regulate a positive feedback loop, in which it triggers resolvins and then acts downstream of them to get things back in order after inflammation clears.
Perhaps the most novel finding of the paper, was what the researchers have termed the "location principle." In their earlier studies, they had found Del-1 secreted from endothelial cells that line tissues was responsible for regulating initiation of inflammation by inhibiting the traffic of neutrophils. But other work has shown that macrophages, too, could secrete Del-1. Using mice that overexpressed either the endothelial-derived Del-1 or the macrophage-derived Del-1, they found that the cell type mattered when it came to the protein's activity. Overexpressing Del-1 only in endothelial cells, for example, made no difference in the animals' ability to clear dying neutrophils in a model of peritonitis. Conversely, mice overexpressing Del-1 in their macrophages had no advantage in harnessing neutrophil recruitment but were better able to clear the neutrophils from the site of inflammation.
"This 'location principle' is novel," says Hajishengallis. "Tissues are not a sack of molecules; the geography is very important.
"As a pro-resolution protein, Del-1 is probably acting downstream of therapeutics that promote periodontal health," he adds. "For instance, the complement inhibitor AMY-101, which can cause a rise in Del-1 levels, may depend on Del-1 to accelerate the resolution of inflammation."
"This fundamental mechanism of inflammation clearance by Del-1," says Chavakis, "may also be involved in multiple inflammatory pathologies, including metabolic-inflammatory or malignant disease."
More information: Ioannis Kourtzelis et al, DEL-1 promotes macrophage efferocytosis and clearance of inflammation, Nature Immunology (2018). DOI: 10.1038/s41590-018-0249-1




















