Study paves way for faster, more accurate therapies for hard-to-treat leukemia patients
A new study will enable clinicians to identify patients with aggressive leukemia who will not respond to chemotherapy and those who are most likely to benefit from a new immunotherapy.
The international research—led by Nottingham Trent University—has involved developing a greater understanding of how the immune system responds in patients with acute myeloid leukemia.
It is hoped that the findings will pave the way for new and more personalized therapies for patients, as well as ensuring they get the right treatment as quickly as possible and without the use of chemotherapy, which is still the standard of care for most individuals with cancer.
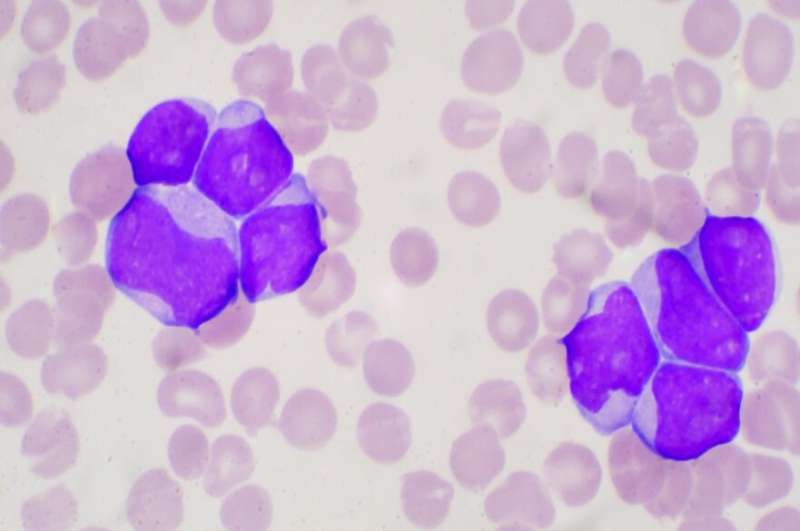
Acute myeloid leukemia progresses quickly, aggressively and requires immediate treatment—it is very resistant to chemotherapy, has a high relapse rate and just one in five patients survive beyond five years of their diagnosis.
The ability to predict the groups of patients and the types of cancer that will respond to immune targeting, an approach that harnesses the body's own immune system to fight cancer, remains limited.
For those that don't respond well to chemotherapy there is a survival rate of just four months and there is currently no treatment for this group.
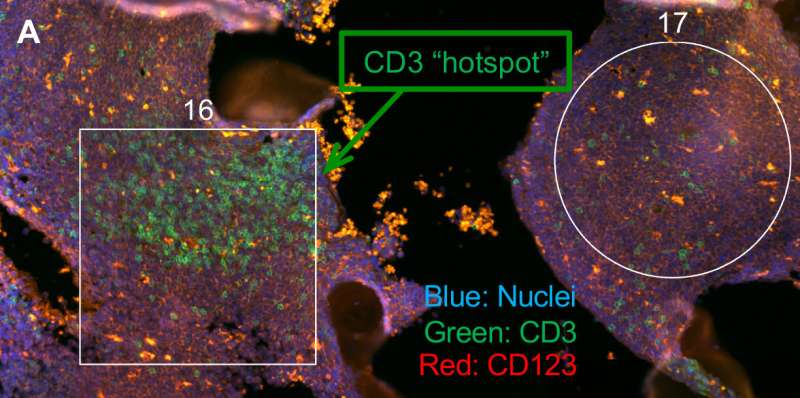
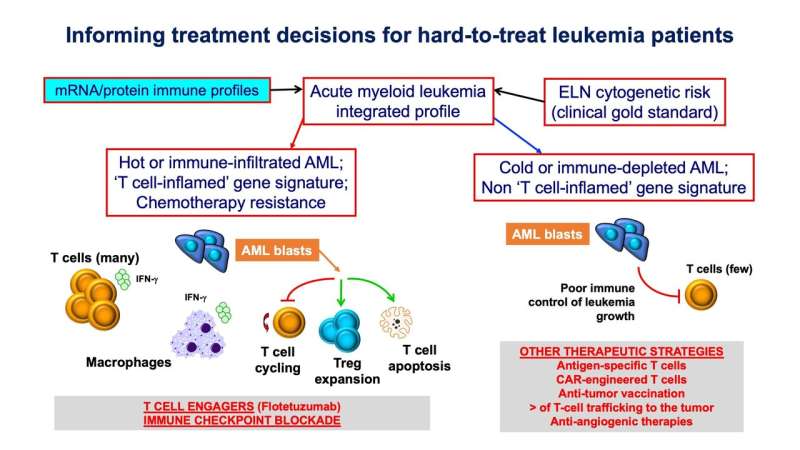
As part of the study the researchers analyzed the immunological structure of bone marrow samples of hundreds of adults and children with AML using innovative technological approaches. This allowed them to unravel critical differences in immune genes across different disease stages and age groups.
The work involved creating a compendium of significant AML genes and proteins to provide new insight into the interactions between patients' immune systems and cancer cells.
This makes it possible to understand how treatment can be tailored to specific patient groups.
The approach led to the identification of immune biomarkers that were able to predict patients who are resistant to chemotherapy and those likely to benefit from flotetuzumab, a new immunotherapy which is currently being developed.
This class of drugs, called "bispecifics", have a similar structure to that of an antibody, and reinvigorate T cells, a subset of immune cells that are normally implicated in the defense against invading microbes and tumor cells and that do not work properly in patients with cancer. Flotetuzumab is designed to bring T cells in close proximity to the tumor cells and promotes their killing.
-

Deciphering the complexity of the immune architecture of acute myeloid leukemia. Credit: Sergio Rutella, Nottingham Trent University -
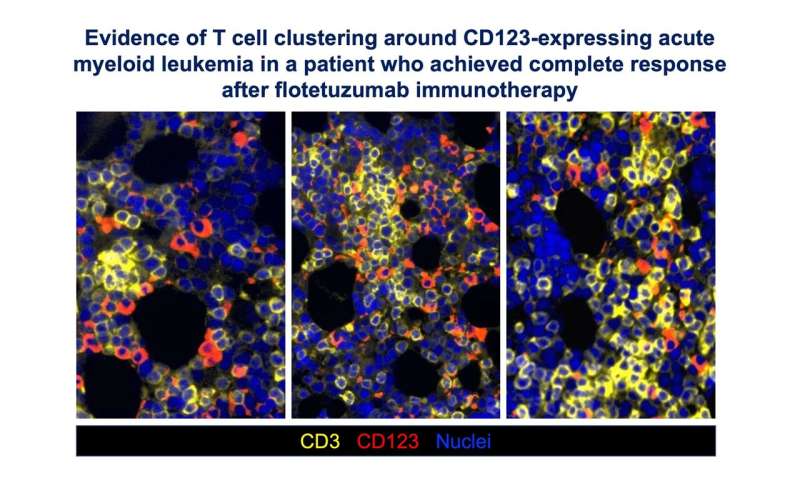
Evidence of T-cell clustering around CD123-expressing acute myeloid leukemia in a patient who achieved complete response after flotetuzumab immunotherapy. Credit: Sergio Rutella, Nottingham Trent University
"Acute myeloid leukemia is an area of unmet clinical need," said Sergio Rutella, Professor of Cancer Immunotherapy in Nottingham Trent University's John van Geest Cancer Research Centre.
He said: "Patient outcomes are unsatisfactory, with chemotherapy resistance and disease recurrence being very common. Our work has characterized the 'immune ecosystem' of AML at unprecedented depth and identified immune gene signatures in the tumor that reflect immune status and predict anti-leukemia immune potential.
"This has transformed our understanding of how treatment should be tailored to specific patients, particularly those resistant to chemotherapy and who are very challenging to treat but could show meaningful responses to second-line immunotherapy with flotetuzumab.
"Being able to predict patient responses will be crucial to tailoring drugs to individuals that are most likely to benefit."
The study, published in Science Translational Medicine, involved clinical hematologists, pathologists, clinical trialists and tumor immunologists.
More information: Jayakumar Vadakekolathu et al. Immune landscapes predict chemotherapy resistance and immunotherapy response in acute myeloid leukemia, Science Translational Medicine (2020). DOI: 10.1126/scitranslmed.aaz0463


















