US regulators seek advice on thorny issues as vaccines near
With vaccines against COVID-19 inching closer, U.S. regulators took an unusual step Thursday in asking outside scientists: Are the government's standards high enough to adequately judge the shots?
The Food and Drug Administration may have to decide by year's end whether to allow use of the first vaccines against the coronavirus, amid growing public fears that politics are overriding science. Thursday, a federal advisory committee pulled back the curtain on that decision process in daylong discussions to be sure corners aren't cut.
"Vaccine development can be expedited. However, I want to stress that it cannot—and must not—be rushed," Dr. Marion Gruber, director of FDA's vaccine research office, told the advisers.
Gruber said the public scrutiny "is critical to build trust and confidence" in whichever vaccines emerge.
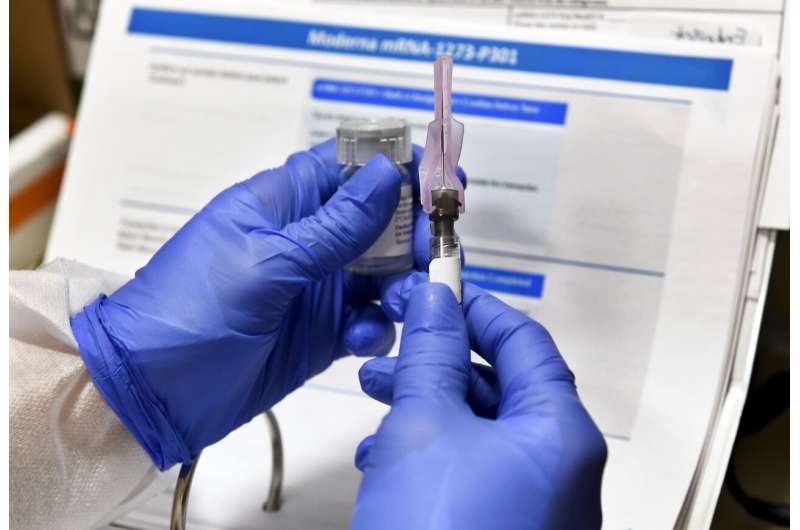
Exactly how much data FDA needs to be sure a vaccine is safe and effective is a key question for the advisers, and one looming as a key vaccine developer, Moderna Inc., announced Thursday the final study of its shot has completed enrollment.
An even tougher question: If the FDA allows emergency use of a vaccine before final testing is finished, will that destroy chances of ever learning just how well those shots—and maybe competitors still being studied—really work?
Any vaccine allowed for emergency use will still be experimental. It may not be clear if the first vaccines prevent people from spreading the coronavirus or just from getting seriously ill, for example. And with multiple shots in the pipeline—made with different technologies that each have pros and cons—the first may not be the best.
FDA's Dr. Doran Fink made clear the agency wants vaccine makers to keep as many volunteers enrolled in their studies for as long as possible to determine long-term vaccine safety and effectiveness.
"Once a decision is made to unblind an ongoing placebo-controlled trial, that decision cannot be walked back and that controlled follow-up is lost forever," Fink said. But asked how to avoid losing that crucial information, he acknowledged: "I don't have any specific remedies to offer at this time."
Thursday's meeting wasn't to evaluate any particular shots. The FDA has pledged to reconvene its advisers to publicly analyze every vaccine before the agency decides its fate.
But it was an opportunity for the FDA to try and assure the public that science-driven vetting of COVID-19 vaccines is happening despite political pressure from the Trump administration and the unprecedented speed at which the shots are being researched. That confidence will be critical to efforts to vaccinate millions of Americans. A recent poll by the Associated Press shows only 46% of those surveyed want to get a COVID-19 vaccine and another 29% are unsure.
Interest was so high, FDA aired the meeting on YouTube.
Some key issues on the committee's agenda:
HOW MUCH EVIDENCE IS NEEDED?
FDA is requiring manufacturers to do studies of at least 30,000 people to prove if a vaccine protects and how safe it is. Those studies must include adequate numbers of people at highest risk from COVID-19—older adults, minorities and anyone with other health problems.
FDA has made clear that any vaccine must be at least 50% effective. And while the studies are designed to run for two years, companies may get enough evidence the shots are protective—in at least some people—to stop the trials early and seek what's called an "emergency use authorization" for wider vaccinations.
Despite White House objections, the FDA told vaccine makers earlier this month not to seek that speedier review until they've tracked at least half their trial volunteers for two months. With other vaccines, that's about the amount of time when major side effects crop up.

And safety questions are growing as two of the four vaccines in final testing in the U.S., one made by AstraZeneca and the other by Johnson & Johnson, are temporarily halted to investigate possible side effects.
Those halts should be reassuring that the process works, said Dr. Hilary Marston of the National Institutes of Health: "We are finding these events because we are specifically looking for them."
But that two-month follow-up period for side effect tracking isn't long enough, said the head of the non-profit ECRI Institute, which reviews medical technology for hospitals and insurers. In comments submitted to the advisory committee, ECRI's Dr. Marcus Schabacker said FDA should require six months of follow-up.
"Doing any less would simply risk too much, and the consequences may be severe," he wrote. "A weak vaccine that loses public trust could poison the well for epidemic control for many years."
Moderna said Thursday that more than two-thirds of its trial participants had received their second dose and were working toward that two-month tracking. The company said it included sufficient groups that have borne the brunt of COVID-19: About a quarter of volunteers are over age 65, and 47% are from minority communities including more than 6,000 Hispanic and more than 3,000 Black participants.
WOULD EMERGENCY USE DERAIL FULL ANSWERS?
Normally when a study ends because of evidence that a vaccine is working, the participants who got dummy shots are offered the real thing.
But if FDA allows emergency use of a COVID-19 vaccine and participants in the placebo group are immediately offered the real shot, researchers may not be able to get answers about all the high-risk groups in the study—or tell how long the vaccine's protection lasts, a process expected to take many more months.
But Pfizer Inc., which with Germany's BioNTech is developing one of the leading candidates, told FDA that if it's granted emergency use authorization, it "would have an ethical obligation" to alert study volunteers who got a placebo and allow them vaccine access. The company wants FDA to look into "other scientifically and statistically sound methods" to determine long-term safety and effectiveness.
Pfizer's stance is likely to face pushback. The Infectious Diseases Society of America states that FDA's panelists "should insist" that vaccine developers "present a compelling case" for how they will complete their trials if FDA grants early authorization of their vaccine.
Clearing a vaccine based on premature or faulty data "could cause more harm" by "further eroding public confidence in all vaccines," the group said.
It's an unprecedented dilemma. The FDA has previously allowed emergency use of only one vaccine, a decades-old shot that in 2005 was authorized to prevent anthrax poisoning.
This time around, multiple coronavirus vaccines are in the pipeline. Pfizer competitor Johnson & Johnson cautioned that early FDA clearance of one vaccine could "jeopardize integrity" of other ongoing trials if participants decide to drop out to seek the first cleared shot instead.
WHAT ABOUT LONG-TERM SAFETY MONITORING?
Even a study of 30,000 people cannot spot a side effect that only strikes 1 in 100,000. So the government is planning extra scrutiny of every COVID-19 vaccine to hit the market.
At first there will be limited doses given to just certain high-risk people—and those early recipients are to get text messages daily for the first week after vaccination, and then weekly out to six weeks, asking how they're feeling.
FDA also will be checking databases of electronic health records and insurance claims, looking for any red flags.
© 2020 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.





















