Disruption in lung cell repair may underlie ARDS in COVID-19 and other diseases
Investigators studying lung cells have discovered that the normal repair process that occurs after lung disease or injury appears to be incomplete but still ongoing in patients who died of COVID-19 and non-COVID acute respiratory distress syndrome (ARDS). In patients who survive but develop scarring in the lungs, it appears that the repair process is permanently arrested, leading to chronic fibrotic lung disease. These findings may lead to novel therapies to promote healthy regeneration to increase survival and prevent fibrosis, they report in The American Journal of Pathology.
"We wanted to understand whether incomplete or impaired repair of the damaged lung might contribute to the high mortality rates from COVID-19 and non-COVID ARDS," explained lead investigator Rachel L. Zemans, MD, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine and Program in Cellular and Molecular Biology, School of Medicine, University of Michigan, Ann Arbor, MI, U.S. "We also wanted to understand why some survivors of ARDS from COVID-19 have normal lungs but others have scarring that leads to lifelong symptoms."
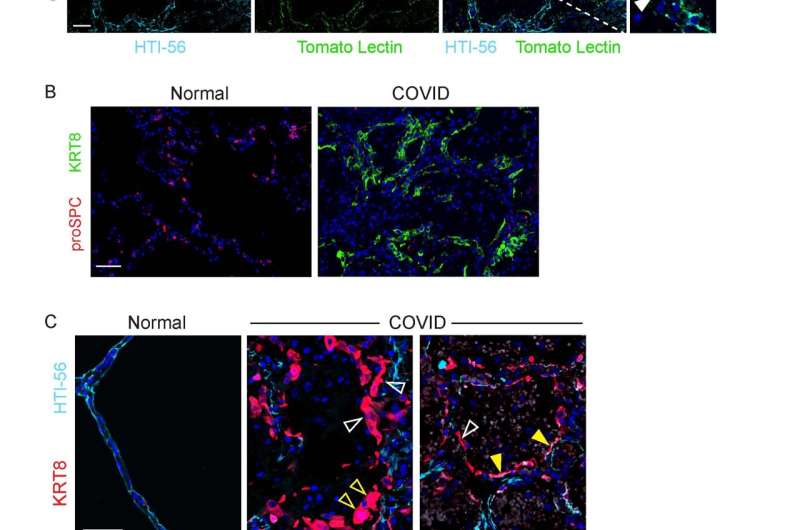
The alveolar epithelium in the lungs is made up of two types of cells. Type 1 alveolar epithelial cells (AEC1) are flat and broad and cover most of the alveolar surface. They play a critical role in barrier integrity and facilitate efficient oxygen absorption. Type 2 alveolar endothelial cells (AEC2) are small cuboidal cells that cover the rest of the surface. They produce a pulmonary surfactant to inflate the lungs and remove fluid. AEC1 and AEC2 are damaged in ARDS due to COVID-19 or other causes. It is known that during lung injury in mice, AEC2 proliferate, exit the cell cycle, and enter a transitional state before changing into AEC1 to repair the alveolar epithelium. In humans with idiopathic pulmonary fibrosis (IPF), AEC2 never leave the transitional state, and change into AEC1, leading to the development of scar tissue known as fibrosis. The state of epithelial injury and regeneration in COVID-19 and non-COVID-19 ARDS without fibrosis had not been well characterized.
The investigators recovered lung tissue from the autopsies of patients who died of COVID-19 or non-COVID-19 ARDS within two weeks of hospitalization. They were compared with patients with IPF. The tissue was examined for evidence of AEC2 proliferation, transitional cells, AEC1 differentiation, indications of the loss of the ability to divide (senescence), and fibrosis. Investigators also compared the gene expression profiles of transitional cells in two mouse models of physiological regeneration without fibrosis, early human COVID-19 and non-COVID-19 ARDS, and human IPF.
The early ARDS lungs had extensive epithelial damage and a regenerative response in which ACE2 proliferated and entered the transitional state. The transitional cells occasionally assumed a flat AEC1 morphology but rarely expressed AEC1 markers. In contrast to patients with IPF, these lungs had not yet developed fibrosis.
"It appears that the stem cells that repair the lungs are able to begin the repair process and assume a 'transitional' or intermediate state," said Dr. Zemans. "However, they have not completely regenerated the cells that were damaged during the injury, leading to acute respiratory failure."
The investigators propose that in COVID-19 survivors who recover normal lungs, the transitional cells do ultimately regenerate the cells that were damaged. However, in survivors who develop scarred lungs, AEC1 are never regenerated; cells are stuck in the transitional state which can lead to scarring and lifelong respiratory impairment.
In an accompanying commentary, Thomas R. Martin, MD, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington School of Medicine, Seattle, WA, U.S., observed, "The COVID-19 pandemic has focused attention on severe lung injury, and this new work uses COVID-19 cases to generate a new perspective on lung injury and repair in ARDS. The results could provide clues about new therapeutic approaches to promote normal repair and/or prevent fibrosis. The results also could be useful in evaluating whether currently available therapies for chronic fibrosis might be helpful early after the onset of acute lung injury."
The study's first author Christopher Ting, MD, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Michigan, added, "As a pulmonary and critical care fellow training during COVID-19, I have seen the pandemic highlight a disease process that we have made frustratingly slow progress on. I hope that pursuing the questions our work poses will continue to shed light on how the lung may heal or not heal after injury."
More information: Christopher Ting et al, Fatal COVID-19 and Non–COVID-19 Acute Respiratory Distress Syndrome Is Associated with Incomplete Alveolar Type 1 Epithelial Cell Differentiation from the Transitional State without Fibrosis, The American Journal of Pathology (2021). DOI: 10.1016/j.ajpath.2021.11.014
Thomas R. Martin, Lung Injury and Repair in Coronavirus Disease 2019–Related Acute Lung Injury, The American Journal of Pathology (2022). DOI: 10.1016/j.ajpath.2022.01.001




















