Multiple sclerosis patients with higher B cell counts found to have a better vaccine response
Multiple sclerosis (MS) patients treated with Rituximab have better responses to the COVID-19 vaccine if they have higher B cell counts. This is the finding of a study from Uppsala University published in the journal JAMA Network Open. In patients with B cell counts of 40/µL (microlitres) or more, 9 of 10 patients developed protective levels of antibodies, while significantly fewer with lower counts had similar responses.
"In our study, the B cell level in patients given Rituximab was the only factor that influenced the ability to form antibodies after vaccination. Previously, it was assumed that it was enough to wait a certain period after administering Rituximab for the vaccine to have a good effect. But to increase the chance of the vaccine causing the body to form antibodies, you first need to measure the level of B cells and ensure there are enough," says Andreas Tolf, a doctoral student in experimental neurology at Uppsala University and physician at Uppsala University Hospital.
In Sweden, Rituximab is the most common medicine for MS, but it is also used for many other diseases. The medicine is given as a drip, normally once or twice a year, and has a documented good effect on slowing the progression of MS. The treatment knocks out the body's B cells, which are an important part of our immune system though they also contribute to the MS disease process. As a result, the treatment increases the risk of patients suffering from serious infections, such as COVID-19. Having low levels of B cells also makes it more difficult for the body to form protective antibodies against viruses and bacteria, which is the primary purpose of vaccinations. In this case, this concerns the S protein in the SARS-CoV-19 virus.
Researchers at Uppsala University and Uppsala University Hospital have studied how MS patients treated with Rituximab react to vaccination against COVID-19. The purpose was to determine the optimal level of B cells for the patient to form sufficient numbers of antibodies after vaccination.
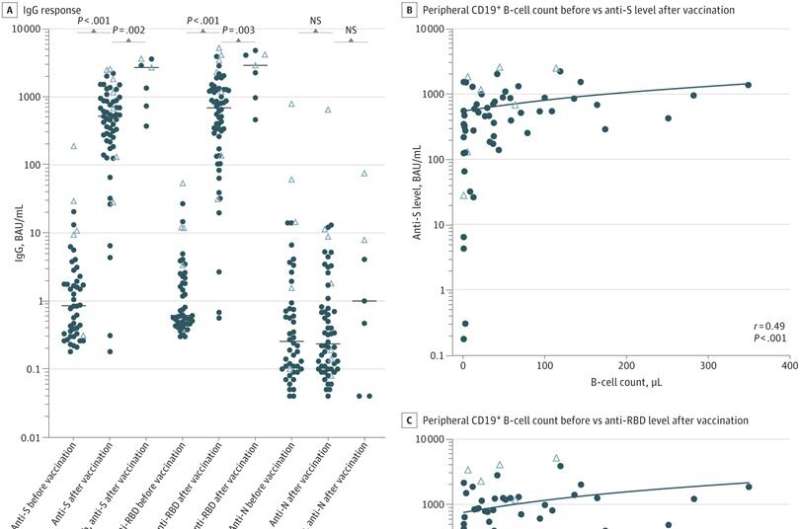
Blood from a total of 67 individuals with MS was analyzed, of whom 60 were undergoing treatment with Rituximab and 7 were going to begin treatment after their COVID-19 vaccinations. Blood samples were taken before and after vaccination to study the levels of B cells and antibodies for SARS-CoV-2. The patients received two doses of Pfizer's COVID-19 vaccine Comirnaty, with the active substance tozinameran.
The results show that the levels of B cells varied greatly among the subjects. The longer a patient had been treated with Rituximab, the longer it took their B cells to recover. For some patients, it took over a year before the B cells began to come back.
The patients who responded best to the vaccine and formed sufficiently high levels of antibodies had on average 51 B cells per microlitre (µL) before the vaccination. For the group that did not reach sufficient levels, the average was 22 B cells/µL.
"There was a threshold with a level of B cells at 40/µL or more where 90 percent formed protective levels of antibodies. Of the patients who were undergoing MS treatment with Rituximab, 72 percent formed sufficiently high levels of antibodies. The best effect with the highest percentage of antibodies was found in subjects who had never been treated with Rituximab," says Anna Wiberg, a researcher in clinical immunology at the Department of Immunology, Genetics and Pathology at Uppsala University.
The researchers have also studied the ability of T cells to react to the virus. No differences were found between subjects who had been treated with Rituximab and those who had never been treated.
The ability of the T cells to react to the virus was just as strong in those who had received treatment. The levels of B cells before vaccination also did not impact the T-cell response, which suggests that all patients have a certain benefit from the vaccination, even if antibodies are not formed.
More information: Andreas Tolf et al, Factors Associated With Serological Response to SARS-CoV-2 Vaccination in Patients With Multiple Sclerosis Treated With Rituximab, JAMA Network Open (2022). DOI: 10.1001/jamanetworkopen.2022.11497




















