Origins of germ cell tumors suggest possible opportunities for future treatment
Researchers have studied the root of germ cell tumors and revealed molecular signatures that could help guide the course of treatment in the future. New research has detailed the origins of germ cell tumors, which are derived from the cells that give rise to sperm or eggs. The results shed light on how these tumors develop, and reveal possible future avenues for novel therapies.
Scientists from the Wellcome Sanger Institute, Cambridge University Hospitals NHS Foundation Trust, and collaborators, uncovered that even though these tumors appear at different ages and can contain multiple cell types, their mutational origins can often be traced back to a genetic event that happened in the womb. In addition to this, these tumors utilize similar pathways of growth as normal tissues that could represent a potential target for treatment.
The research, published 11 August 2022 in Nature Communications, also observed that tumors which develop before puberty carry distinct patterns of mutations, known as mutational signatures. While further investigation is needed, these could be used in the future to help inform clinical decisions when it comes to treating children with germ cell tumors.
Malignant germ cell tumors can appear at any age and are one of the most common cancers of adolescent and young men. They also account for 5% of all childhood cancers, with around 45 children being diagnosed every year in the U.K.
Germ cell tumors can be made up from a variety of cell types, including muscle, placenta or teeth and hair in some cases. The cell types that the tumor is composed of has implications for the prognosis, as some can be more aggressive than others. This study looked at how these tissues develop together within tumors, and contrasts them with how healthy tissues grow, which has not previously been possible.
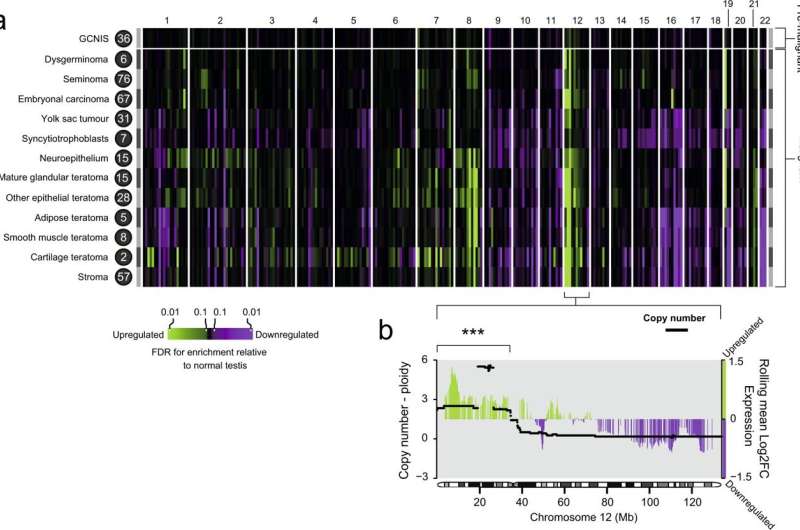
In this new research, scientists from the Wellcome Sanger Institute, Cambridge University Hospitals NHS Foundation Trust, and their collaborators, examined tumor samples from 15 individuals. By applying in-depth genetic sequencing techniques, they were able to study the DNA and RNA of all the different tissues they sampled within the tumors at an unprecedented resolution.
By analyzing this extensive amount of genetic information, the team were able to trace the origin of the tumors all the way back to the beginning of their development in the womb. They found that the way tumors created tissues, such as cartilage or muscle, shared similarities with how those are created in a growing embryo which may represent novel treatment targets.
The researchers also identified different mutational signatures in tumors of young children compared with tumor samples taken from older children, over the age of 12. Therefore, the mutational signatures the team found could be used as a future biomarker that allows healthcare professionals to identify which course of chemotherapy is the most appropriate based on the cancer's genetic makeup. This could prove particularly useful for children who develop these tumors around the current age cut-offs which determine the treatment they receive.
"We are excited to find genetic features that can be used to distinguish the tumors so clearly. Clinically, treating teenage and young adult patients can be challenging as they fall between pediatric and adult treatment protocols. It is important to treat them sufficiently but not excessively to avoid long-term side effects, so getting the intensity of the chemotherapy right is important. Our research suggests that the genetic makeup of the tumor might be used to help categorize such patients, which will hopefully result in children, and indeed all patients with germ cell tumors, getting the most appropriate therapy in the future," says Dr. Thomas Oliver,
co-first author from the Wellcome Sanger Institute and Cambridge University Hospitals NHS Foundation Trust.
"Germ cell tumors can be made up of a variety of different tissues, including smooth muscle and skin, and previously very little was known about the factors behind their development, making them difficult to understand and treat. Our research has shown that these tumors can be traced back to the same genetic event, and the tissue types have developed from different branches of the same family tree, shedding more light on how these tumors are formed," says Dr. Raheleh Rahbari, co-senior author from the Wellcome Sanger Institute.
"Germ cell tumors affect around 45 children in the U.K. every year. However, they can also develop at any age. Interestingly, our research found that early development signals, those which you see while a fetus is developing in the womb, can be found in these tumors. In the future, it may be possible to target these, as is done in some blood cancers, to give a new type of therapy for those with this type of cancer," says Dr. Sam Behjati, co-senior author from the Wellcome Sanger Institute and Cambridge University Hospitals NHS Foundation Trust.
Max Williamson, now 24, was diagnosed with testicular cancer at Bedford Hospital when he was 15 years old. Max said, "I noticed a growing lump which was worrying, and when I went to my GP I was quickly referred to my local hospital which gave me my diagnosis. I had no history of cancer in my family. I was then referred to Cambridge University Hospitals NHS Foundation Trust for treatment. Whilst an operation removed the primary cancer, it rapidly spread to the lymph nodes in my abdomen and I had to undergo three courses of chemotherapy.
"For me, an important part of experiencing cancer was trying to answer questions like 'Why me?' 'What happened to this part of my body to cause cancer?' Nine years on, it's so great to see the Cambridge team who looked after me (and many other researchers across the world) continuing to answer this question."
Professor Matthew Murray, co-author on the paper and co-chair of the Biology Committee for the Malignant Germ Cell International Consortium, said, "Max had a malignant germ cell tumor, which is the leading adult cause for average years of life lost per person dying of cancer. When Max's tumor changed from localized to metastatic—with the rapid spread to his lymph nodes—his treatment had to be urgently changed from follow-up surveillance to chemotherapy.
"This study, which analyzed both the DNA and RNA, found little relationship between the tissues the tumor made—what we can see down the microscope—and the changes found in the genetic code. Clearly, the tissue's appearance doesn't tell the whole story and underlines the needs for additional molecular tests that can accurately predict a tumor's behavior. The genetic patterns observed in this study are also a significant step forward in our understanding of these tumors, which, with more research, will aim to improve and personalize treatment of this type of cancer for patients like Max."
More information: Thomas R. W. Oliver et al, Clonal diversification and histogenesis of malignant germ cell tumours, Nature Communications (2022). DOI: 10.1038/s41467-022-31375-4

















