This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Researchers find immune response to COVID strengthens over time
Immunity from COVID-19 appears to gather strength with more time between vaccination and infection, a new laboratory study from researchers at Oregon Health & Science University suggests. The findings carry implications for vaccine recommendations as the pandemic transitions to an endemic state.
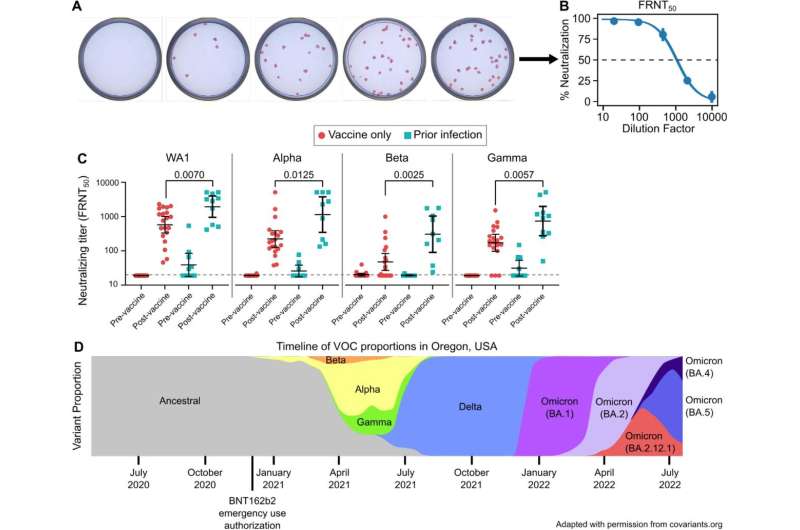
Researchers measured the antibody response in blood samples for a group of people who gained so-called "hybrid immunity" through two means: either vaccination followed by a breakthrough infection, or by getting vaccinated after contracting COVID-19. They measured the immune response in blood samples of 96 generally healthy OHSU employees and found that the immune response was uniformly stronger the longer the time period between vaccination and infection. The longest interval measured was 404 days.
Their findings suggest that vaccine boosters should be spaced no more frequently than a year apart, at least among healthy people.
"Longer intervals between natural infection and vaccination appear to strengthen immune response for otherwise healthy people," said co-senior author Fikadu Tafesse, Ph.D., associate professor of molecular microbiology and immunology in the OHSU School of Medicine.
The study comes as an advisory panel for the Food and Drug Administration is due to meet Thursday, Jan. 26, to consider the nation's COVID-19 vaccine strategy going forward.
Published in the Journal for Clinical Investigation Insight, the new research is the latest in a series of laboratory discoveries by OHSU scientists revealing a pattern of strengthened immune response through hybrid immunity. Their findings suggest that the magnitude, potency and breadth of hybrid immune response all increased with a longer time period between exposure to the virus—whether through vaccination or natural infection.
This likely is related to the body's immune response maturing over time, said co-senior author Marcel Curlin, M.D., associate professor of medicine (infectious diseases) in the OHSU School of Medicine and medical director of OHSU Occupational Health.
"The immune system is learning," Curlin said. "If you're going to amplify a response, what this study tells us is that you might want to boost that response after a longer period of learning rather than early after exposure."
Further, the research team found that it didn't matter whether someone developed hybrid immunity by getting vaccinated after contracting COVID-19 or after a breakthrough infection following vaccination. Both groups developed an equally potent immune response.
The findings suggest long-lasting potency of so-called "memory cells," the B cells that recognize an invading virus and generate protein antibodies to neutralize the virus and its many variants. The authors write that an ever-growing pool of people who have contracted the SARS-CoV-2 virus stand to benefit from vaccination, even if they've delayed it until now.
Relying on natural infection alone is a bad idea, "given the risks of severe illness, long-term complications, and death," the authors write.
The researchers say the findings are the latest to point toward the virus evolving to an endemic state.
"Our results point to a future where inevitable vaccine breakthrough infections would be expected to help build a reservoir of population-level immunity that can help blunt future waves and reduce the opportunity for further viral evolution," they write.
The researchers cautioned that the immune response was measured in relatively healthy people, and boosters may be advisable on a more frequent basis among vulnerable people who are older or are immunocompromised.
More information: Timothy A. Bates et al, The time between vaccination and infection impacts immunity against SARS-CoV-2 variants, medRxiv (2023). DOI: 10.1101/2023.01.02.23284120
Timothy A. Bates et al, An extended interval between vaccination and infection enhances hybrid immunity against SARS-CoV-2 variants, JCI Insight (2023). DOI: 10.1172/jci.insight.165265 , insight.jci.org/articles/view/165265


















