This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
proofread
Rising rates of benzodiazepine toxicity among young people spark concern
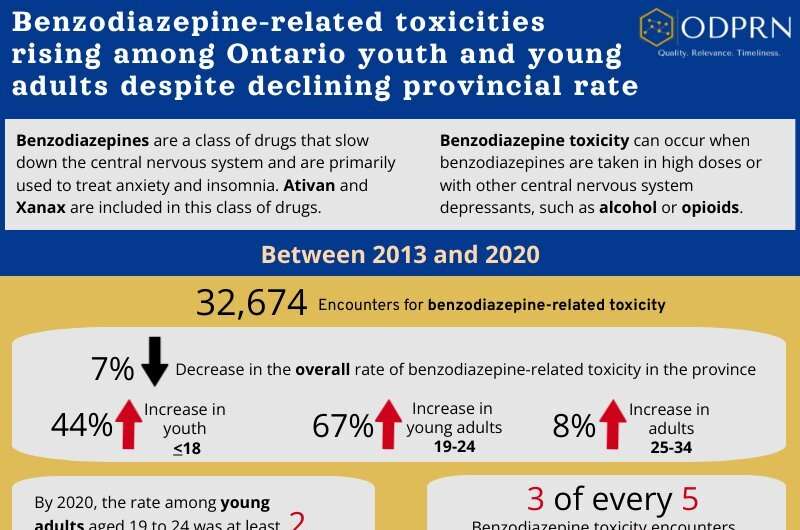
The rate of hospital encounters for benzodiazepine-related toxicity rose by 67% for young adults (aged 19 to 24) and 44% for youth (aged 18 or below) in Ontario between 2013 and 2020, according to a new study from ICES and Unity Health Toronto.
Though there was an overall decline of 7% in the provincial rate of benzodiazepine toxicity, this was largely driven by reductions in rates among people aged 35 years and older.
Benzodiazepines are commonly prescribed to treat anxiety and insomnia, but in recent years they have also emerged in the unregulated and illicit opioid drug supply.
The study was published in the Canadian Journal of Public Health and facilitated by researchers at the Ontario Drug Policy Research Network (ODPRN), housed at St. Michael's Hospital, a site of Unity Health Toronto. A Citizens' Panel made up of 25 volunteer citizens identified the topic as being of interest to the public and was involved in all steps of the research process.
"As a member of the ODPRN Citizens' Panel, we were initially drawn to the gap in information about benzodiazepine toxicity specifically relating to the youth and young adult population," says panel member Josephine Quercia.
"Outside of the older adult population, studies were nonexistent specific to the younger age group. Our interest was further peaked by the significant increase in prescribing rates among this younger population and especially among the female population within this segment. What initially started as a potentially positive outcome with the '7% reduction in the provincial rate of benzodiazepine toxicity between 2013—2020," once unpacked, pivoted quickly to a very different outcome—one where focus is needed on reducing the risks to our youth and young adult population."
The study included 25,979 Ontario residents with 32,674 benzodiazepine-related toxicity encounters (emergency department visits or hospitalization) between January 1, 2013, and December 31, 2020. The researchers also examined the participants' history of opioid and benzodiazepine prescriptions, and prior healthcare visits for mental health and substance use disorders.
"Importantly, we also found that fewer encounters were with patients who had an active prescription for benzodiazepines—however, there was greater involvement of other substances, such as opioids, stimulants, and alcohol, with rates of those incidents reaching almost 30% in 2020," says lead author Tonya Campbell, senior research coordinator at St. Michael's Hospital. "This is likely driven by the increasing presence of non-pharmaceutical benzodiazepines in the unregulated drug supply in Ontario."
Study findings show:
- Rates of benzodiazepine toxicity rose substantially for young adults aged 19-24 (67% increase, from 40 to 67 per 100,000) and youth aged 18 or below (44% increase from 11 to 16 per 100,000 population).
- The percent of encounters in which patients had an active benzodiazepine prescription declined over the study period, from 61% in 2013 to 49% in 2020.
- In 2020, 29% of benzodiazepine toxicity incidents also had an opioid-, alcohol-, or stimulant-related toxicity documented on the encounter, of which opioid involvement was most common (17%).
- Almost 50% of people who experienced benzodiazepine toxicity had a hospital encounter for a mental health or substance use disorder in the year prior, of which anxiety disorders (19%) and mood disorders (19%) were the most common reasons.
"Taken together, these trends are concerning, and likely reflect the continued risks for youth and young adults prescribed benzodiazepines as well as the recent arrival of these drugs in the unregulated opioid supply in Ontario," says senior author Dr. Tara Gomes, a scientist at the Li Ka Shing Knowledge Institute of St. Michael's Hospital and ICES, and a principal investigator of the ODPRN. "Therefore, we need a comprehensive response that includes improved access to community-based mental health services, a focus on the safe use of prescription benzodiazepines, and alternatives to the unpredictable unregulated opioid drug supply."
One limitation of the study is that data were unavailable for incidents that went untreated or were treated outside of a hospital, and drug screening practices across emergency departments vary. This means that rates of benzodiazepine toxicity were likely underreported in this study. Furthermore, the researchers did not examine characteristics or patterns of intent, meaning whether toxicity events were accidental or related to self-harm.
Nevertheless, this is the first study to examine long-term trends and patterns of benzodiazepine-related toxicity in Ontario and is consistent with findings that demonstrate rising rates of benzodiazepine-related harm across North America.
The study, "The epidemiology of benzodiazepine-related toxicity in Ontario, Canada: a population-based descriptive study" was published in the Canadian Journal of Public Health.
More information: The epidemiology of benzodiazepine-related toxicity in Ontario, Canada: a population-based descriptive study, Canadian Journal of Public Health (2023). DOI: 10.17269/s41997-023-00784-3





















