This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Maternal vitamin D deficiency found to increase lifetime diabetes risk in offspring
Researchers at Washington University School of Medicine in St. Louis have identified a process in immune cells that links vitamin D deficiency during pregnancy to an increased risk of type 2 diabetes in offspring. The researchers also found that these immune cells and their embedded genes can be used to transfer type 2 diabetes into otherwise healthy mice. The research is published June 13 in Nature Communications.
Some theories of disease suggest that conditions in utero may have irreversible, lifelong consequences in offspring. The new study's principal investigator, Carlos Bernal-Mizrachi, MD, said that could be happening to the children of mothers who don't have adequate levels of vitamin D during pregnancy.
"The identification of modifiable, environmental risk factors that may contribute to the later development of metabolic diseases is critical to prevent and treat those diseases," said Bernal-Mizrachi, a professor of medicine in the Division of Endocrinology, Metabolism & Lipid Research. "As the incidence of diabetes and prediabetes has tripled in recent decades, particularly in children and young adults, we are analyzing environmental conditions during pregnancy that may help explain the increase."
About 37 million Americans have been diagnosed with diabetes, and at least 98 million more have prediabetes, a condition marked by the body's resistance to insulin. Vitamin D deficiency during pregnancy, a deficiency that affects an estimated 80% of Black American women and 60% of Caucasian women, may be one of the factors contributing to insulin resistance and elevated risk for diabetes in offspring.
"In studies of mice born to vitamin D-deficient mothers, we have found that the animals go on to develop insulin resistance and diabetes later in life," Bernal-Mizrachi said. "That was true even when pups were treated with adequate amounts of vitamin D after birth. Those animals improved their glucose control, but they never normalized."
The researchers have identified a type of stem cell that may be irreversibly affected by vitamin D deficiency during development in utero. The stem cells develop into immune cells, and the researchers discovered that they could transplant diabetes into other animals by placing these stem cells into mice with normal vitamin D levels. The researchers concluded that insufficient levels of vitamin D in utero can program the immune cells to promote the development of diabetes, providing a target to potentially prevent this process.
In those experiments, the researchers found that the immune cells activated a genetic process that is the same such process activated in immune cells collected from delivering mothers who had insufficient vitamin D levels when they gave birth.
Although prenatal vitamins are prescribed to ensure adequate levels of key nutrients during pregnancy, these findings from Bernal-Mizarachi and his colleagues suggest that the recommended doses of vitamin D are not sufficient to normalize vitamin D levels in women who had low vitamin D levels prior to pregnancy.
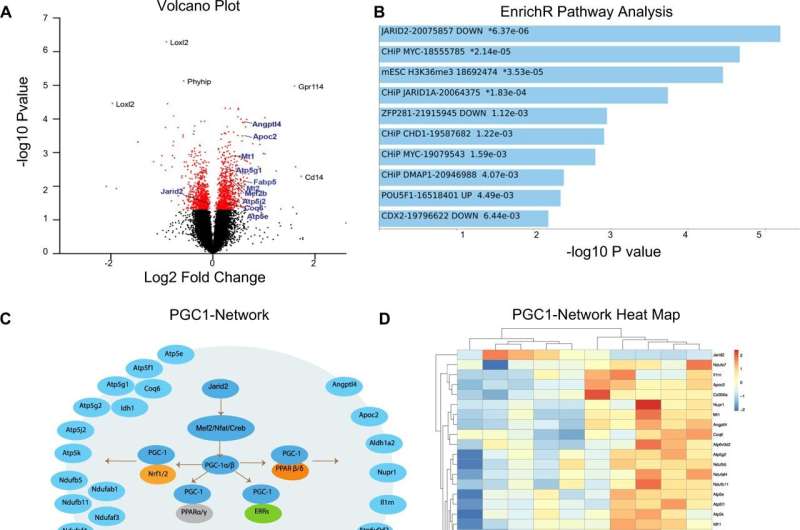
The process the researchers identified in mouse fetuses was characterized by alterations in specific genes. The modified gene program was identified in the stem cells that later developed into immune cells, including macrophages. The research team discovered that these macrophages secrete a molecule that impairs the ability of fat tissue to store glucose, resulting in increased blood sugar levels.
"Macrophages that come from vitamin D-deficient stem cells get into the fat tissue and contribute to inflammation, causing the fat tissue to become insulin resistant," said Bernal-Mizrachi, who also is chief of medicine at the Veterans Affairs St. Louis Health Care System.
Importantly, the researchers found evidence that the same processes that promote inflammation and insulin resistance in fat tissue also are at work in people. Immune cells isolated from cord blood from vitamin D-deficient pregnant patients who were cared for by physicians at Washington University showed similar changes in immune cell genes and secreted molecules that had been identified previously in mice.
More information: Jisu Oh et al, Embryonic vitamin D deficiency programs hematopoietic stem cells to induce type 2 diabetes, Nature Communications (2023). DOI: 10.1038/s41467-023-38849-z




















