This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New testing method offers better diagnosis and treatment for the most severe form of male infertility
Researchers have uncovered two proteins that are unique to viable sperm, offering men with the most severe form of male infertility both a non-invasive diagnostic test and more information about their chances to one day become a parent through in vitro fertilization.
About 15% of couples experience infertility, roughly half due to male infertility, says lead author Andrei Drabovich, a biochemist and assistant professor of laboratory medicine and pathology at the University of Alberta.
Some males have no or low sperm count in their semen because of an obstruction, while about 2% don't produce enough viable spermatozoa for traditional insemination, a condition known as non-obstructive azoospermia. Treatment involves a complex surgery that can take many hours to dissect the testes in search of intact sperm, which are then frozen for later use with in vitro fertilization.
The two proteins will facilitate development of a new diagnostic test to predict whether that surgery is likely to be successful, and would help surgeons identify viable sperm during the surgery, says Drabovich.
"The routine semen tests typically show zero sperm in non-obstructive azoospermia, but is it really zero? With our approach we are able to record a million images and in some patients find only 10 spermatozoa. But even a few would be enough for in vitro fertilization," he says.
"Knowing that would benefit patients in their decision-making and help surgeons."
A decade of work to better understand male infertility
Drabovich began his research on male infertility when he was a postdoctoral fellow a decade ago and continues to collaborate with researchers at Mount Sinai Hospital and the University of Toronto. The team first identified proteins to diagnose whether azoospermia is obstructive or non-obstructive.
Their studies used an advanced technique of mass spectrometry and revealed thousands of specialized proteins that are unique to the male reproductive system. While the function of most proteins is not fully understood, some are involved with sperm movement, some with cell metabolism and others with fertilization.
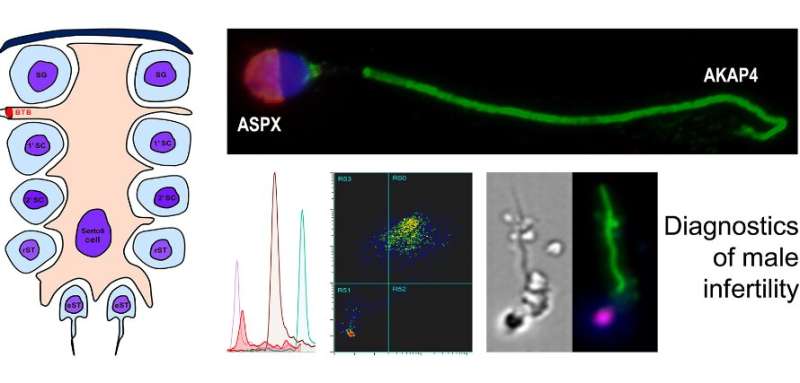
To follow up on those studies, Drabovich and colleagues used specialized techniques and equipment to identify cells in semen that have the telltale elongated shape of sperm and the target proteins on both the head and the tail.
"The final test will use a very comprehensive technique of imaging flow cytometry to measure a signal from each protein and also take an image," he explains. "Getting all these levels of information at the same time helps us filter a million images and detect even a single viable spermatozoon."
Drabovich's laboratory will continue work to understand the function of the spermatozoa proteins, including looking for ones which could be turned off temporarily as a potential method of non-hormonal, reversible male contraception. Drabovich's lab is also focused on finding biomarkers for aggressive prostate cancer and new ways to measure antibodies against viruses such as COVID-19.
More information: Junyan Zhang et al, Germ Cell–Specific Proteins AKAP4 and ASPX Facilitate Identification of Rare Spermatozoa in Non-Obstructive Azoospermia, Molecular & Cellular Proteomics (2023). DOI: 10.1016/j.mcpro.2023.100556




















