This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Research explains the role of high cholesterol in SARS-CoV-2 infectivity
A recent study has unveiled the doorway that SARS-CoV2 uses to slip inside cells undetected.
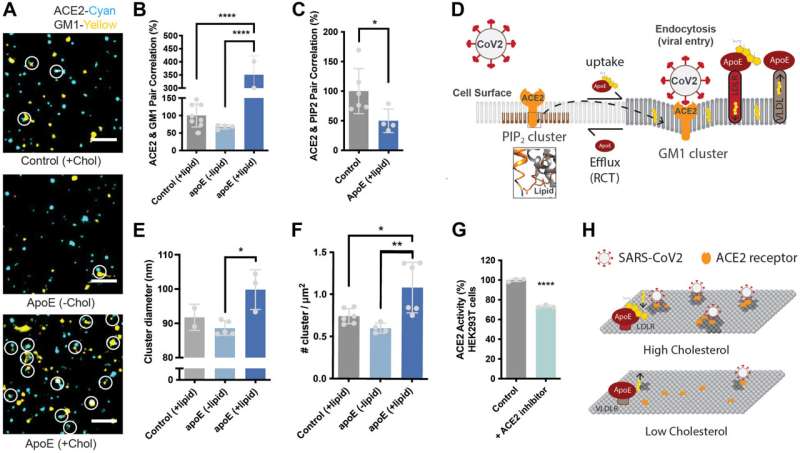
SARS-CoV-2 uses the receptor angiotensin-converting enzyme 2, or ACE2, to infect human cells. However, this receptor alone does not paint a complete picture of how the virus enters cells. ACE2 is like a doorknob; when SARS-CoV-2 grabs it and maneuvers it precisely, this allows the virus to open a doorway to the cell's interworking and step inside, but the identity of the door has eluded scientists.
Scott Hansen, an associate professor of molecular medicine at the University of Florida Scripps, discovered that cholesterol clusters make up that door. His team published their work in the Journal of Biological Chemistry.
Early on in the COVID-19 pandemic, the elderly and people with chronic diseases such as hypertension, diabetes, Alzheimer's and cardiovascular diseases experienced more viral-related deaths. However, children seemed to be less susceptible.
Hansen hypothesized that part of this phenomenon was due to the high amounts of tissue cholesterol in populations with chronic disease. From 2017 to 2020, 86.4 million U.S. adults age 20 or older had high or borderline high cholesterol in the blood.
After completing studies using cutting-edge technology like super resolution microscopy, his team showed that cholesterol on the cell surface makes ACE2 readily accessible to SARS-CoV2 for cell entry.
"Our cells have a protective coat of lipids, or fat, that keeps out invaders and bad molecules," Hansen said. "Cholesterol is a part of a place where nutrients come into the cell. I live in Florida; so we think of this mechanism as, if a hurricane is coming, you batten down the hatches after collecting resources. But this virus is sneaking in when you pull the door closed."
Cholesterol is necessary for survival, but too much cholesterol may be increasing your risk for COVID-19 at the cellular and biochemical levels.
"In smokers with chronic disease, cholesterol in the lung tissue is elevated two-fold, a magnitude of change that dramatically increases infectivity of the virus in cell culture," Hansen said. In fact, according to a study, supported by the National Heart, Lung, and Blood Institute, smoking was associated with a higher risk of severe COVID-19, including death.
However, Hansen's past research has shown that the cholesterol promoting SARS-CoV-2 infection can easily be disrupted to help patients stay healthy and avoid infection.
"Mechanical force and polyunsaturated fatty acids disrupt the aggregation of the cholesterol," Hansen said. "Healthy mechanical force is achieved with exercise. In our studies, cells need to be jostled a little bit in order to keep the cholesterol from setting up in the cell membrane. Regular exercise with its increased heart rate and blood flow should reduce the cholesterol aggregates in the cell membranes."
In addition to new insights on the entry mechanism of SARS-CoV-2, Hansen's study also highlighted the inaccuracies of the way doctors assess cholesterol risk in their patients. Currently, the only way to test cholesterol levels is via a blood test.
"Basically, cholesterol goes both ways," Hansen said. "It gets loaded into cells, which is the forward pathway. But then there's reverse cholesterol transport where the body takes cholesterol back out of the cells and moves it to your liver and excretes it out of the body or recycles it. If you measure cholesterol levels in the blood, you don't know the levels in the tissue or if it is being taken out or brought in."
Hansen and his team are working with physicians to come up with a test that more accurately represents tissue cholesterol and its distribution throughout the body.
"In the future, this study may affect how doctors think about cholesterol in the body," Hansen said. "Instead of focusing on the blood, which changes every time you eat, they will need to focus on the tissues and how the cholesterol is taken up over time. It's a harder measurement, but, in the end, it may help people understand their risk for disease and save lives."
More information: Hao Wang et al, The role of high cholesterol in SARS-CoV-2 infectivity, Journal of Biological Chemistry (2023). DOI: 10.1016/j.jbc.2023.104763




















