This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study uncovers role of ultraviolet radiation in development of rare leukemia in the skin
A change of scenery can restore one's outlook, but for some precancerous cells, a journey from the caves of the bone marrow to the sunny climes of the skin can trigger genetic changes that are a harbinger of cancer, according to a new study by researchers at Dana-Farber Cancer Institute, Brigham and Women's Hospital, and the Broad Institute of MIT and Harvard.
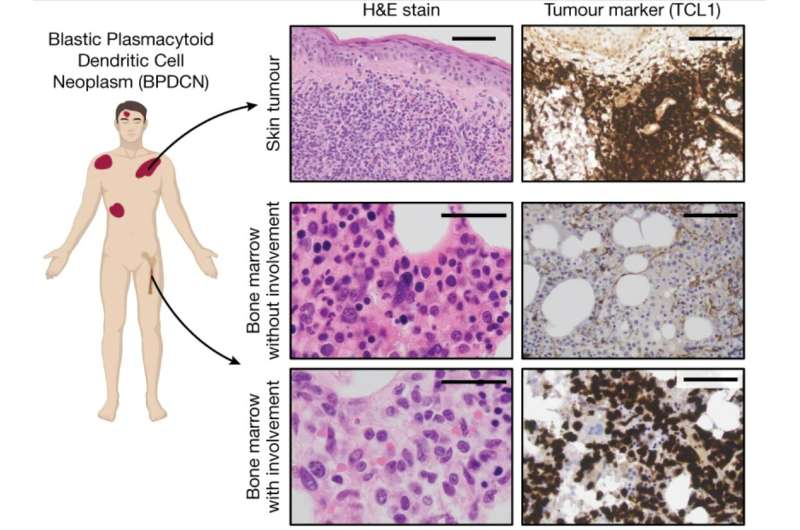
The study, published online today by the journal Nature, is one of the first to uncover the "genetic travelog" of a cancer that evolves across multiple different tissues. Although it focused on a rare form of cancer—blastic plasmacytoid dendritic cell neoplasm (BPDCN)—the research may shed light on how other cancers develop, particularly those involving blood or lymph cells that travel the bloodstream to all corners of the body, investigators say.
"The cells within our body live in very different environments depending on which organ or tissue they're in," says study co-senior author Andrew Lane, MD, Ph.D., of Dana-Farber and the Broad Institute. "In this study, we demonstrate how exposure to more than one of these environments can shape the evolution of premalignant cells to tumor cells."
"The results add to our understanding of the development of BPDCN, which is critical to devising new and better treatments for the disease," he continues. "They may also be applicable to any cancer that evolves in more than one site—and potentially to how cancers change after they've metastasized to other parts of the body."
BPDCN is an aggressive malignancy of the bone marrow and blood that is diagnosed in 200-400 people in the United States each year, usually in patients 60 or older, and more often in men than women. It is also something of an anomaly among leukemias.
"At the time patients first come to medical attention, about half of them have tumors of leukemia cells in their skin, but when we examine their bone marrow, blood, or lymph nodes—where we'd expect to find leukemia cells—we don't see anything abnormal," says Lane, director of the BPDCN Center at Dana-Farber. "The other half have skin tumors as well as leukemia cells in the more traditional places."
The symptoms of the first group of patients are puzzling because, according to the model of how leukemia progresses, cancerous cells first appear in the bone marrow, then travel via the blood to other parts of the body, including the skin. The fact that these patients had skin lesions but, apparently, normal marrow defied that model.
Lane and his colleagues sought to solve the conundrum by collecting samples of bone marrow and skin tumors from 16 patients, including those whose bone marrow looked normal, and analyzing the cells for genetic mutations.
In patients whose only sign of disease was in the skin, researchers found that the ostensibly normal bone marrow cells had mutations that matched some of the mutations of the leukemia cells in the skin. This suggests that BPDCN begins in the bone marrow as a condition called clonal hematopoiesis (CH)—in cells that harbor mutations but behave normally—and shows up in the skin as leukemia cells with additional mutations.
To better understand this process, researchers did a deep dive into the genetics of patients' bone marrow, blood, and skin leukemia cells—sequencing the DNA and RNA in individual cells.
"We wanted to determine which cells in the bone marrow and blood are acquiring these initial mutations, and which cells are accruing the mutations we see in the skin leukemia tumors," Lane explains.
To accomplish this, the researchers developed a new technological approach they called eXpressed Variant sequencing (XV-seq) that integrates two powerful forms of genetic analysis, single-cell gene expression and genotyping.
"We needed a high-resolution view into how these tumors were evolving, so that we could see which mutations arose early in disease, which ones appeared later, and in which cells," said study co-senior author Peter van Galen, Ph.D., of Brigham and Women's Hospital and the Broad. "XV-seq allowed us to precisely identify mutation-carrying cells and pinpoint rare circulating malignant cells that standard clinical approaches couldn't see."
They found that all the patients had blood and bone marrow cells with early CH mutations. They then identified the culprit for the added mutations in the skin leukemias: the sun—specifically, ultraviolet rays in sunlight.
"We found that in the tumors in the skin—and in leukemia tissue from blood and bone marrow—the leukemia cells had mutations caused by ultraviolet [UV] radiation," Lane remarks. (Scientists have mapped the specific patterns of gene mutations produced by UV light.) "In some patients, a single CH cell in the bloodstream had to have been exposed to ultraviolet radiation—and picked up additional mutations—before it could become a leukemia cell."
Researchers could now plot the develop of BPDCN in the skin in three steps: 1) Bone marrow cells develop mutations for clonal hematopoiesis; 2) At least one of those cells, venturing into the skin, acquires mutations from UV light; 3) The cell later incurs other mutations that turn it into a full-fledged leukemia cell.
To buttress this account of the disease's origins, the investigators enlisted dermatological researchers to determine where patients' skin lesions first formed. "We found that almost all of them occurred in sun-exposed areas," Lane relates. "In other types of leukemia that can invade the skin, the lesions are randomly distributed across the skin. Our findings strongly suggest that skin exposure to UV rays, and the resulting genetic mutations, are part of the process of this disease."
Lastly, researchers explored how the most common gene mutation in BPDCN affects the development of the disease. The mutation, in the gene Tet2, is found in 80% of patients with BPDCN, many of whom have alterations in both copies of the gene, completely shutting it down.
In a series of experiments, researchers found that when the normal counterparts of BPDCN cells are exposed to ultraviolet light, they die. When BPDCN cells carrying Tet2 mutations are put under the same light, they survive. "This may explain why so many BPDCN cells withstand ultraviolet radiation exposure in the skin, which gives them the opportunity to acquire more mutations and become leukemic," Lane remarks.
More information: Andrew Lane, Ultraviolet radiation shapes dendritic cell leukemia transformation in the skin, Nature (2023). DOI: 10.1038/s41586-023-06156-8. www.nature.com/articles/s41586-023-06156-8





















