This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New vaccine technology produces more antibodies against SARS-CoV-2 in mice
A new technology developed at Caltech is designed to make more potent vaccines, beginning with SARS-CoV-2 (the virus that causes COVID-19). In mouse studies, the prototype vaccine elicited five times more antibodies than current COVID-19 vaccines. The antibodies produced by the new vaccine were effective against the original strain of SARS-CoV-2, the delta variant, and omicron variants.
The new vaccine candidate has been dubbed a "hybrid" vaccine because it combines features of mRNA technology that is used by the Pfizer and Moderna vaccines with features of protein nanoparticle-based vaccines, such as the Novavax shot. In addition to assisting the fight against COVID-19, the technology could one day improve vaccines for HIV, influenza, and myriad other pathogens.
The research was conducted in the laboratory of Pamela Björkman, the David Baltimore Professor of Biology and Biological Engineering and Merkin Institute Professor. The study was led by Magnus Hoffmann (Ph.D. '22), who will start an independent laboratory as a Merkin Institute Fellow at the Merkin Institute for Translational Research at Caltech. The paper titled "ESCRT recruitment to SARS-CoV-2 spike induces virus-like particles that improve mRNA vaccines," appears in the journal Cell.
"For any vaccination or infection, antibody levels contract over time," says Björkman. "The ideal vaccine would produce a potent immune response that elicits high levels of antibodies that mitigate infection by multiple variants of a virus and cytotoxic T cell responses that kill infected cells to protect against severe disease and death."
Vaccines teach the immune system how to recognize and fight a specific pathogen, but there are multiple ways to do so. Current vaccines for SARS-CoV-2 teach the immune system to recognize the virus's spike protein—the protein on the virus's surface that enables it to grasp and enter human cells—either by providing the body with the protein's genetic material (its mRNA) or with fragments of the protein itself. The new vaccine candidate is a hybrid technology that combines both mRNA and protein-based strategies. In mouse studies, only two immunizations were required to produce robust antibody levels against Omicron-based variants, as opposed to three with traditional COVID-19 vaccines.
"During a natural infection, the immune system encounters both infected cells and free virus particles," says Hoffmann, who received Caltech's Milton and Francis Clauser Doctoral Prize for his Ph.D. thesis on this work. "Current mRNA vaccines mimic infected cells, while protein nanoparticle-based vaccines mimic free virus particles to stimulate immune responses. Our hybrid technology does both."
"The Merkin Institute is focused on seeding and accelerating the translation of research from Caltech labs," says Caltech's Barbara Wold (Ph.D. '78), Bren Professor of Molecular Biology, and director and Allen V. C. Davis and Lenabelle Davis Leadership Chair of the Richard N. Merkin Institute for Translational Research. "As our first Merkin Fellow, Magnus now leads a lab advancing the development of EABR technology. It's an innovative approach that builds on what's known about existing cellular mechanisms to strengthen and more accurately tailor immune responses. From this starting point, Magnus and his new group can look forward to optimizing and then extending the hybrid approach. While there is much yet to do, if all goes well, they will ultimately realize the promise of more effective and durable vaccines for multiple human diseases. That's the home run."
Vaccines and beyond: Unpacking the EABR technology
The study's major breakthrough is a new technology that engineers membrane proteins, such as the SARS-CoV-2 spike protein, to induce the formation of virus-like nanoparticles that bud off from the cell membrane by utilizing existing aspects of cellular machinery. With this particular application, the technology was used for developing vaccines, but it can be applied for myriad research purposes.
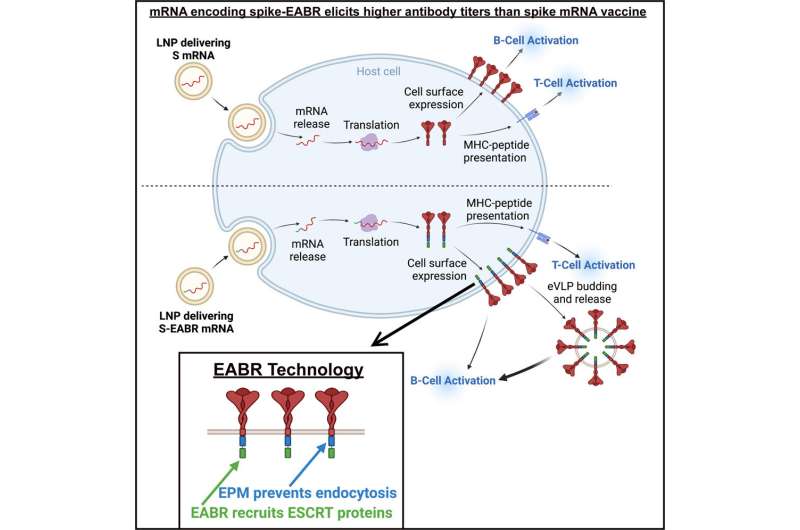
To understand how the new technology—called EABR (ESCRT-and ALIX-binding region) technology—produces a better vaccine against COVID-19, it is useful to understand how current vaccine technologies work.
mRNA vaccines contain the genetic material that encodes the SARS-CoV-2 spike protein, and they work by inducing your own cells to produce harmless pieces of the protein. These pieces are produced by vaccinated person's own protein synthesis machinery to stick out of the surface of a subset of their cells, alerting the body's immune cells to recognize a SARS-CoV-2 virus through both B cells that produce antibodies that can neutralize the virus and T cells that can destroy infected cells.
On the other hand, protein-based vaccines contain pieces of the spike protein itself and deliver them directly into your body, where they circulate freely. Like with an mRNA vaccine, the immune system springs into action, creating antibodies that precisely fit the shape of the protein and teaching immune cells how to recognize it.
The new vaccine, based on EABR technology, is similar to an mRNA vaccine, in that it contains genetic material encoding for the SARS-CoV-2 spike protein. After injection, cells take in the mRNA and begin using their own machinery to churn out protein pieces.
However, the hybrid technology also incorporates additional little "tails" onto these pieces. These tails activate a series of natural cellular processes (called the ESCRT pathway) that enable the pieces to clump together to form nano-sized spiky balls, or "virus-like particles." While some spike protein pieces stay on the surface of the cell as in a traditional mRNA vaccine, the virus-like particles bud off from the cell and circulate through the body in the same way that protein-based vaccine nanoparticles do.
EABR technology to build self-assembling nanoparticles could be useful for myriad different research purposes other than developing vaccines, including the nanoparticle-based delivery of therapeutics to specific target cells such as cancer cells. Multiple Caltech laboratories are collaborating with the team to use EABR technology for various studies.
More information: Magnus A.G. Hoffmann et al, ESCRT recruitment to SARS-CoV-2 spike induces virus-like particles that improve mRNA vaccines, Cell (2023). DOI: 10.1016/j.cell.2023.04.024





















