This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
The long-term course of severe long COVID: Study tracks patients with pronounced fatigue over 20 months
A new study from Charité-Universitätsmedizin Berlin and the Max Delbrück Center has found that many people with post-COVID syndrome who suffer from fatigue six months after a coronavirus infection are still severely physically impaired up to 20 months afterward.
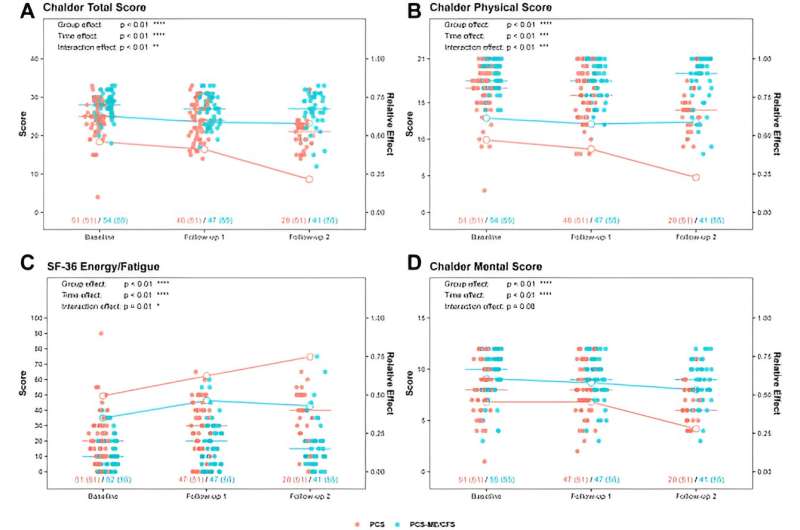
The vast majority of patients who develop myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) remain severely ill, with no change. By contrast, patients with similar symptoms who do not meet the diagnostic criteria for ME/CFS experience gradual improvement in their symptoms. The study has been published in the journal eClinicalMedicine.
Patients who still have health problems three months after a SARS-CoV-2 infection, with symptoms ongoing for at least two months and no other explanation for these issues, are said to have post-COVID syndrome (PCS), also known as "long COVID." Symptoms vary widely.
Many people have problems with breathing, trouble concentrating, or little to no stamina. A large portion of people with PCS complain of fatigue that barely improves with normal rest and recovery. In many cases, these people struggle to cope with daily life, and even slight exertion exacerbates their condition, a phenomenon known as exertion intolerance. This situation is significantly more common in women than men.
Patients and others are naturally wondering how long these symptoms will persist. Findings from a number of studies are now available for the initial few months following infection. According to this research, recovery generally takes longer the more severe the initial infection was. Many people—but unfortunately not all—see symptoms improve within a year. The long-term progression of the illness in these patients has been unclear so far.
How long is the shadow cast by COVID-19?
The study that has just been published focuses on people who still suffer from severe fatigue and exertion intolerance six months after contracting SARS-CoV-2. In contrast to studies based solely on patients' descriptions of their symptoms, this study involved a comprehensive medical examination on the 106 participants—most of them women—at three points in time at several-month intervals.
"Unfortunately, our data show that people with post-COVID syndrome who have severe fatigue are still ill more than a year and a half after the initial infection," says Dr. Judith Bellmann-Strobl, the study's last author and a senior physician with the Neuroimmunology Outpatient Clinic at the Experimental and Clinical Research Center (ECRC), a joint institution of Charité and the Max Delbrück Center. "Only half of them—the half that do not present with the full range of symptoms of ME/CFS—experience gradual improvement in at least some symptoms."
Two groups of PCS patients with severe fatigue and exertion intolerance
Researchers had observed last year that long COVID sufferers with severe fatigue and exertion intolerance fall within two groups. Some of the patients meet the diagnostic criteria for ME/CFS, a complex neuroimmunological disease with the key symptoms of severe fatigue, exertion intolerance and post-exertional aggravation of symptoms that can lead to physical disability. Patients in the second group experience similar symptoms, but their post-exertion symptoms are generally milder and do not last as long.
The new study shows that the latter group experiences some improvement over time, not only in fatigue, but also in terms of general malaise, pain, and concentration problems. These people's functional ability often improved, and some of those studied were even able to return to work. By contrast, post-COVID patients with ME/CFS saw barely any change in their symptoms. There were very few exceptions. "Seven of the 55 patients with ME/CFS experienced improvement in their physical impairments," Bellmann-Strobl explains. "But we still don't have an explanation for this, and we haven't been able to identify any medical commonalities."
Grip strength as a guide to prognosis?
Another observation made in the study may be useful going forward in gauging how post-COVID syndrome will progress in people who meet the diagnostic criteria for ME/CFS: The stronger these patients' grip strength was at the start of the disease, the less severe their symptoms were up to 20 months later.
"Grip strength was not only a parameter for how severe the disease was to start with, but also a predictor of how ME/CFS would progress," explains Prof. Carmen Scheibenbogen, Acting Director of the Institute of Medical Immunology at Charité and the head of the Charité Fatigue Center. She and Bellmann-Strobl were the principal investigators in the study. "Before we can use grip strength as a prognostic factor, though, we need further studies to confirm how meaningful it is," Scheibenbogen points out.
"The WHO puts the number of people living with long COVID in Europe at about 36 million right now. Most of them experience impairments in daily life, and many can no longer lead a normal life at all," she explains. "Even before the pandemic, there were an estimated three million people with ME/CFS in Europe, and the data we now have suggest that there are now twice that number due to the pandemic. Our study shows that most people with ME/CFS remain severely ill. In addition to ramping up our efforts to find effective therapies, this means we also need to quickly establish health care facilities where patients can receive multidisciplinary care based on current scientific findings and clinical experience."
In the absence of treatments that do more than just alleviate symptoms and instead go to the root cause of post-COVID syndrome and ME/CFS, Bellmann-Strobl's main recommendation for patients is to pace themselves so they do not exhaust their energy reserves and not to overexert themselves. Tools that can help with this include fitness trackers or pedometers, heart rate monitors, activity journals, and relaxation exercises. "Pacing can prevent post-exertional malaise, a worsening of the person's condition. The better patients do with pacing, the less severe their symptoms. People should be very careful in feeling out their limits in terms of exertion. Professional guidance can help to prevent overexertion."
About ME/CFS
ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) is a severe neurological disease that is typically caused by an infection and often becomes a chronic condition. Its main characteristic is post-exertional malaise, which involves significant exacerbation of symptoms after minor physical or mental exertion. This form of malaise may not develop until several hours later or even the next day and typically lasts until the next day or, in many cases, several days or even longer. It is associated with physical weakness and frequently with headache or muscle aches and also often involves neurocognitive, autonomous, and immunological symptoms.
Before the pandemic, the incidence of ME/CFS at the worldwide population level was estimated at about 0.3%. Experts believe the number of those living with this condition has risen significantly as a result of the COVID-19 pandemic. Pathogens such as Epstein-Barr virus, the influenza virus, the dengue virus, and enteroviruses have been previously identified as triggers of ME/CFS. Many cases of ME/CFS were also observed in people who contracted the first SARS coronavirus in 2002–2003. ME/CFS is distinct from post-viral fatigue, which can last weeks to months following many infectious diseases.
More information: Franziska Legler et al, Long-term symptom severity and clinical biomarkers in post-COVID-19/chronic fatigue syndrome: results from a prospective observational cohort, eClinicalMedicine (2023). DOI: 10.1016/j.eclinm.2023.102146





















