This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Examining the association between low oxygen conditions induced by hyperglycemia and impaired insulin secretion
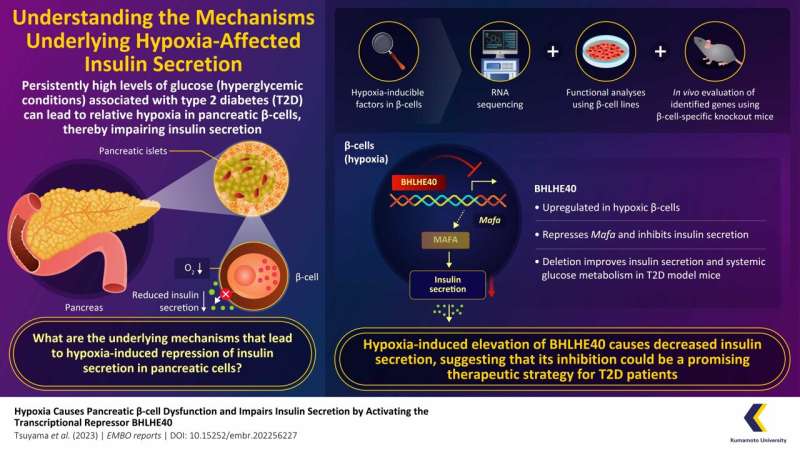
Type 2 diabetes (T2D) is characterized by persistent hyperglycemia (high glucose in blood) that leads to hypoxia (low oxygen condition) in pancreatic β-cells.
Now researchers from Japan have found that levels of BHLHE40, a transcriptional repressor, is greatly increased under these hypoxic conditions, which reduces insulin secretion. They also observed that removal of the gene BHLHE40 in diabetic mice restored insulin secretion. Thus, targeting BHLHE40 could open up new avenues for therapies against T2D. The findings of their study were published on 21 June 2023 in the journal EMBO Reports.
T2D is a chronic metabolic disorder that affects more than 500 million people worldwide. It is characterized by insulin resistance, a condition where the cells of the body fail to respond to insulin, resulting in hyperglycemia. Persistent hyperglycemia has been shown to affect pancreatic β-cells, which are responsible for secreting insulin and maintaining normal glucose levels in the blood, which leads to disruption of insulin secretion.
Previous research has shown that hypoxic conditions are developed within the pancreatic β-cells due to persistent hyperglycemia (as a part of pancreatic β-cell glycotoxicity). These conditions are believed to be caused due to the high dependency of β-cells on oxygen for the production of energy to secrete insulin. This low-oxygen state can have detrimental effects on β-cell function and contribute to the development and progression of T2D. However, the exact mechanism behind such hypoxia-induced β-cell dysfunction is still not fully understood.
To address this issue, a team of researchers led by Professor Kazuya Yamagata and Assistant Professor Tomonori Tsuyama from the Graduate School of Life Sciences at Kumamoto University, Japan deep dived into the nuances of hyperglycemia-induced hypoxia in T2D. "It is known that chronic hyperglycemia caused by insulin resistance in T2D impairs the function of pancreatic β-cells, thereby exacerbating the condition, but little is known about the underlying mechanisms," states Prof. Yamagata.
The researchers first carried out an experiment to understand the impact of hypoxia on global gene expression of human and mice β-cells in order to search for genes whose expression varied in response to the created hypoxic conditions. They discovered that the expression of a gene called BHLHE40 is elevated under hypoxic conditions. This gene codes for the protein BHLHE40 that acts as a "transcriptional repressor," a molecule that reduces the expression of other genes.
The researchers then investigated the role of BHLHE40 in pancreatic β-cells. They found that when it was overexpressed, BHLHE40 impaired insulin secretion by reducing the expression of genes involved in β-cell function, a prominent one among them being musculoaponeurotic fibrosarcoma oncogene family A (MAFA).
Further, in order to confirm their findings in vivo, the researchers removed BHLHE40 gene from a diabetic mouse model. They noted that deletion of BHLHE40 not only restored the expression of MAFA, but also increased insulin secretion and improved the mice's ability to metabolize glucose.
Elucidating the mechanism through which BHLHE40 affects the progression of T2D, the researchers concluded that hyperglycemia-induced glycotoxicity in pancreatic β-cells led to low-oxygen conditions that resulted in increased expression of BHLHE40, followed by the inhibition of MAFA, and the subsequent disruption of insulin secretion.
Restoration of insulin secretion in mice deficient in BHLHE40 confirmed that targeting this gene can reverse β-cell dysfunction and may prove to be a promising candidate for newer therapies against T2D.
Discussing their study, Dr. Tsuyama emphasizes, "These findings provide valuable insights into the molecular mechanisms underlying hypoxia-induced β-cell dysfunction. By targeting the gene BHLHE40, we may be able to develop new therapies aimed at preserving β-cell function and ultimately slow down the progression of T2D."
This research contributes to a better understanding of the development and progression of T2D along with offering promising targets for future therapeutic interventions.
More information: Tomonori Tsuyama et al, Hypoxia causes pancreatic β‐cell dysfunction and impairs insulin secretion by activating the transcriptional repressor BHLHE40, EMBO reports (2023). DOI: 10.15252/embr.202256227




















