This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Stretching and stimulating engineered heart tissues to accurately portray hypertrophic cardiomyopathy
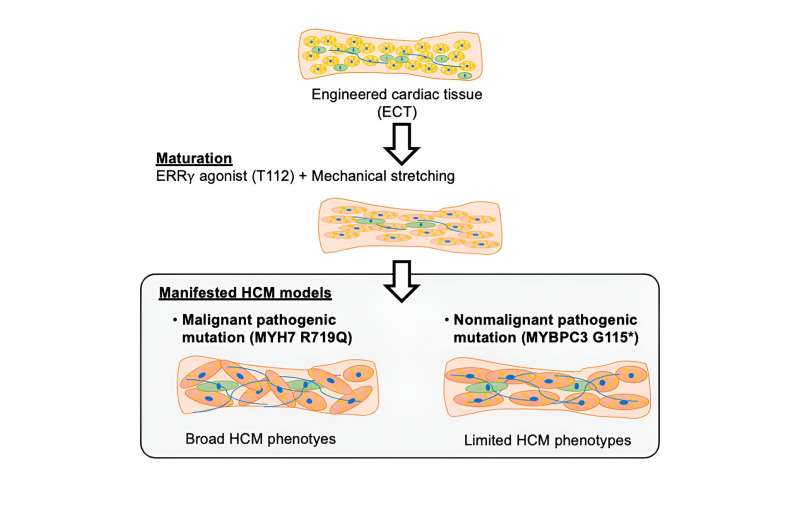
A joint effort by a team of academic and industrial researchers led by Associate Professor Yoshinori Yoshida (Department of Cell Growth and Differentiation) created a new modeling system, combining mechanical stretching and chemical stimulation, to generate mature engineered cardiac tissues (ECTs) and employed them to better model hypertrophic cardiomyopathy.
With next-generation disease modeling, researchers attempt to reproduce disease conditions in Petri dishes using patient-specific induced pluripotent stem cell (iPSC)-derived tissues. However, to accurately model heart diseases, such tissues must reach a maturation stage that faithfully recapitulates adult tissues.
Building upon their previous discovery that showed ERRγ agonist, T112, promotes the metabolic and structural maturation of iPSC-derived cardiomyocytes, the research team additionally incorporated mechanical stretching of the iPSC-derived heart tissue into the maturation protocol and demonstrated the synergistic effects of the combinatorial treatment by metabolic, structural, functional, and transcriptomic evaluations. The findings are published in the journal Stem Cell Reports.
Utilizing this new modified protocol with improved cardiomyocyte maturation, the research team focused on using it for better disease modeling. Hypertrophic cardiomyopathy (HCM) is a condition characterized by the abnormal thickening of the heart muscle forming the left ventricle, caused predominantly by mutations of the sarcomere components, such as myosin heavy chain β (MYH7) or myosin-binding protein C (MYBPC3).
Although the genetics underlying HCM pathology is well-known, there are no curative therapeutic options other than symptomatic treatments, partly due to the difficulty of creating HCM disease models. While there have been reports of HCM animal models, few are particularly useful for understanding the pathogenic mechanism or identifying new therapies due to various species differences between humans and many model organisms. For example, MYH7, the most frequently mutated disease-associated gene, is lowly expressed in adult mouse hearts, thus making data interpretation extremely challenging. Therefore, alternative disease modeling systems are necessary for new advances in understanding and treating HCM.
The researchers thus sought to model HCM caused by two distinct mutations: the severe MYH7 R719Q missense mutation and the milder MYBPC3 G115X nonsense mutation by creating isogenic iPSC lines with these HCM patient-specific mutations by CRISPR/Cas9 genome editing and differentiated them into ECTs using both the basic (no mechanical or chemical stimulation) and modified protocols (mechanical or chemical stimulation only, or both mechanical and chemical stimulation) to determine how combined treatment aids HCM disease modeling.
Remarkably, whereas the basic protocol or chemical stimulation alone failed to distinguish between wild-type (WT) and MYH7 R719Q mutant ECTs in multiple measurements examined, mechanical stimulation alone or the combinatorial protocol discerned clear differences between healthy and disease ECTs. Similarly, MYBPC3 G115X mutant ECTs generated using the combined treatment displayed disease phenotypes that were not apparent in ECTs produced using the basic protocol. Consistent with clinical findings, ECTs with the non-malignant HCM mutation (MYBPC3 G115X) only exhibited a subset of disease phenotypes detected in ECTs modeling malignant HCM (MYH7 R719Q mutation).
Additionally, the researchers performed transcriptome analysis of both mutant ECTs and found gene expression profile changes consistent with clinical samples collected from HCM patients. Specifically, they found gene sets related to contraction, extracellular matrix, fibrosis, and energy metabolism to be significantly altered in the disease ECTs, thus recapitulating the remodeling and functional disruptions of the left ventricle caused by the disease.
With their newly improved differentiation protocol, the research team could reproduce various HCM phenotypes, like hypertrophy, hypercontractility, and diastolic dysfunction, in the disease ECTs. However, it was only with the incorporation of mechanical stretching during the maturation process that additional phenotypes, such as myofibril disarray and fibronectin accumulation, could be observed.
The researchers demonstrated the power and utility of this new maturation method to generate ECTs to accurately capture numerous disease phenotypes that were impossible before this study. They noted that, nonetheless, there remains room to improve upon this work because there are still certain aspects of HCM pathophysiology that their current ECTs are unable to reveal.
The hope is that their continuous efforts to produce progressively better ECTs will soon help to better model HCM pathology to identify suitable treatment strategies or test new therapeutic agents.
More information: Yuya Fujiwara et al, ERRγ agonist under mechanical stretching manifests hypertrophic cardiomyopathy phenotypes of engineered cardiac tissue through maturation, Stem Cell Reports (2023). DOI: 10.1016/j.stemcr.2023.09.003




















