This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Beta-cells study sheds light on cause of type 2 diabetes
Scientists at Johns Hopkins All Children's Hospital, along with an international team of researchers, are shedding new light on the causes of type 2 diabetes. The research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or, perhaps, even prevent type 2 diabetes from developing.
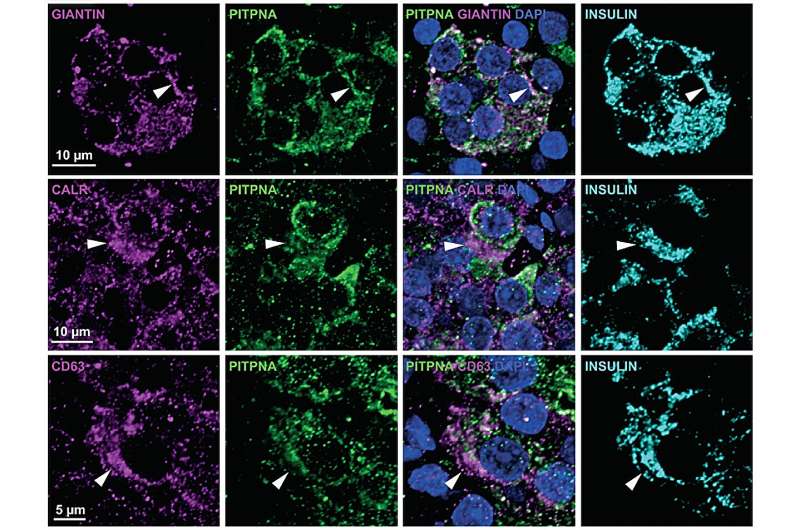
The study shows that the beta-cells of type 2 diabetes patients are deficient in a cell trafficking protein called "phosphatidylinositol transfer protein alpha" (or PITPNA), which can promote the formation of "little packages," or intracellular granules containing insulin.
These structures facilitate processing and maturation of insulin "cargo." By restoring PITPNA in the type 2 deficient beta-cells, production of insulin granule is restored and this reverses many of the deficiencies associated with beta-cell failure and type 2 diabetes.
Researchers say it's important to understand how specific genes regulate pancreatic beta-cell function, including those that mediate insulin granule production and maturation like PITPNA to provide therapeutic options for people.
Matthew Poy, Ph.D., an associate professor of Medicine and Biological Chemistry in the Johns Hopkins University School of Medicine and leader of the Johns Hopkins All Children's team within the Institute for Fundamental Biomedical Research, was lead researcher on the study. He adds that follow-up work is now focused on whether PITPNA can enhance the functionality of stem-cell-derived pancreatic beta-cells.
Since stem cell-based therapies are still in their relatively early stages of clinical development, it appears a great deal of the potential of this approach remains untapped. Poy believes that increasing levels of PITPNA in stem cell-derived beta-cells is an approach that could enhance the ability to produce and release mature insulin prior to transplantation in diabetic subjects.
"Our dream is that increasing PITPNA could improve the efficacy and potency of beta-like stem cells," Poy says. "This is where our research is heading, but we have to discover whether the capacity of these undifferentiated stem cells that can be converted into many different cell types can be optimized—and to what level—to be converted into healthy insulin producing beta-cells. The goal would be to find a cure for type 2 diabetes."
More information: Yu-Te Yeh et al, Restoration of PITPNA in Type 2 diabetic human islets reverses pancreatic beta-cell dysfunction, Nature Communications (2023). DOI: 10.1038/s41467-023-39978-1





















