This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Accelerating drug development for lung diseases: New insights from single-cell genomics
Drug development for lung diseases is complicated. Most clinical trials that test novel drugs fail due to the fact that laboratory models cannot accurately replicate human physiology.
Currently specific molecular pathways are often modeled in highly artificial conditions using one or two different cell types in a culture dish in the laboratory. Such simple systems do not fully replicate the tissue environment of the lung, and therefore these laboratory models are lacking representation of therapeutically relevant cell-cell communication pathways.
Revolutionizing pre-clinical drug development: Organotypic model system for lung research
A new promising experimental model to mechanistically study lung disease emerged recently: so-called human precision-cut lung slices (hPCLS). These are thin sections of lung tissue, that can be used for experiments in the lab.
To generate hPCLS, scientists from Helmholtz Munich work with human lung tissue obtained from patients undergoing surgery due to lung diseases. The tissue gets cut into thin slices that can be kept alive in the lab. hPCLS have the unique advantage of retaining the full cellular diversity and native three-dimensional structure of the lung.
The team of researchers led by Prof. Schiller and Dr. Burgstaller have now performed an in-depth analysis of all cells within the hPCLS, thereby significantly advancing the possibilities and usage of this lung disease model.
They leveraged the power of single-cell genomics, which records gene activities in individual cells, to analyze the activity of all cells in hPCLS after specific experimental and therapeutic treatments.
Understanding treatment response: Insights from human precision-cut lung slices
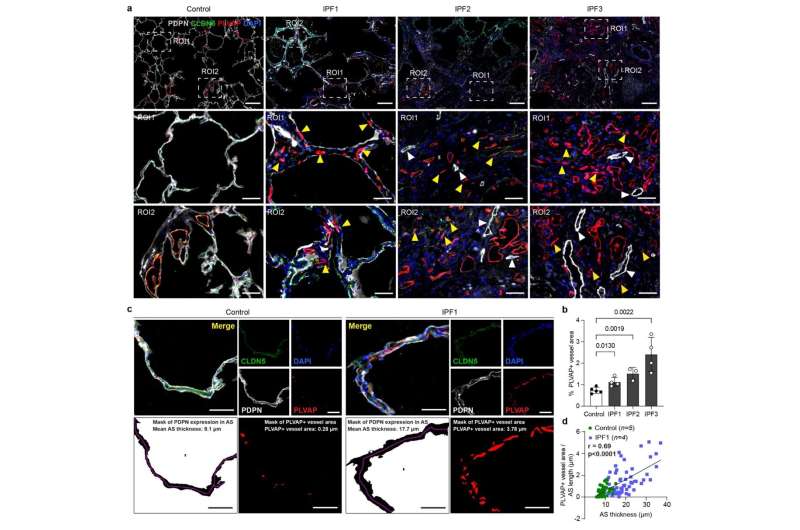
The new advanced knowledge about hPCLS was used by the team to understand how disease-specific cellular activities that occur in lung fibrosis patients can be induced in the hPCLS model system, and how these disease specific cellular states can be affected by different anti-fibrotic drugs.
The authors computationally integrated several single-cell transcriptomic datasets from multiple patient cohorts and used artificial intelligence (AI)-based transfer learning approaches to understand how cell states that were induced by cytokine and drug treatments in the hPCLS model compare to the Human Lung Cell Atlas (HLCA) of health and disease.
The HLCA is a comprehensive map detailing characteristics of all cell types within the human lung and was released earlier this year by Helmholtz Munich scientists and their international partners.
The new methods and insights from this study showcase the power of experimental studies in hPCLS to enable analysis of tissue homeostasis, regeneration and pathology.
Prof. Schiller says, "We are now working on doing these hPCLS perturbation experiments at scale to learn more about the regulation of lung tissue states in health and disease and provide an experimental model for drug testing directly in human lung tissue." Ultimately, these efforts by Helmholtz Munich scientists have the capacity to significantly speed up the development of novel therapies.
The work is published in the journal Science Translational Medicine.
More information: Niklas J. Lang et al, Ex vivo tissue perturbations coupled to single-cell RNA-seq reveal multilineage cell circuit dynamics in human lung fibrogenesis, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.adh0908



















