This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
How an immune response is driven by one letter difference in DNA
A one-letter difference in our DNA determines whether BCG vaccine provides good protection against tuberculosis or not. Researchers at Radboudumc have elucidated how that one-letter difference affects the activation and deactivation of the immune system. The discovery, published in Nature Genetics, not only provides more insight into interleukin-driven inflammatory responses but also opens up new possibilities for (re)guiding the immune system.
People can react very differently to the same pathogen or vaccination. One person gets sick from an invading bacterium, for instance, while another doesn't. And some vaccines work much better on some people than on others. The main reason for these individual differences lies in our genetic material, our genome. A genome differs from person to person. It is this diversity that largely determines how we react to pathogens and vaccinations.
Our complete genome consists of more than 3 billion DNA molecules. In these biological DNA letters, our heredity is stored. Only a small portion of these letters, about 2 percent, contain information about the proteins at work in our bodies. Those proteins are the workforces in our cells; they build us up, repair us, and keep us alive. The 2 percent of the genome that codes for proteins is called the exome. It was long thought the other 98 percent of our DNA was actually redundant. It was genetic waste—"junk DNA" without a function.
Vaccine against tuberculosis
We now know that this junk DNA, hereafter referred to as the non-coding genome, is indeed very important. That 98 percent may not make proteins, but it can help to shape them, coordinate their production and so on. The genome does so by making pieces of RNA. Such a piece of non-coding RNA interferes with all kinds of processes in the body. Including the chance that you will (not) get sick from a pathogen. Or whether or not a vaccine will protect you properly.
Let's take the BCG vaccine that protects against tuberculosis (TB) as an example. This vaccine appears to protect not only against TB, but against more infections by (epigenetic) changes that the vaccine evokes in blood-forming stem cells in the bone marrow.
Different DNA letters, different immune responses
Among other things, those stem cells produce the white blood cells that are important in the immune system. But the BCG vaccine does not work equally well in everyone. It turns out that just one letter difference in the hereditary material drives this distinction. Such a "one-letter difference" is called a single-nucleotide polymorphism, in short SNP, and pronounced as "snip."
In people with the letter G (for guanine) at this place in the genome, vaccination works very well. For people with an A (for adenine), the vaccine works only moderately. Therefore, the question is: how can one letter difference have such an impact on the functioning of a person's immune system?
Musa Mhlanga and Ezio Fok of Radboudumc and their colleagues tried to answer this question. Fok says, "We know that a BCG vaccine activates interleukin-1β. This triggers an inflammatory process through which the immune system builds up protection against tuberculosis and other pathogens. But why does it work really well in people with a G-SNP, and is it less efficient in those with an A-SNP? What exactly happens there in that molecular incubator? Why do those G and A cause such a big difference in the way our immune system functions?"
Director of the inflammatory process
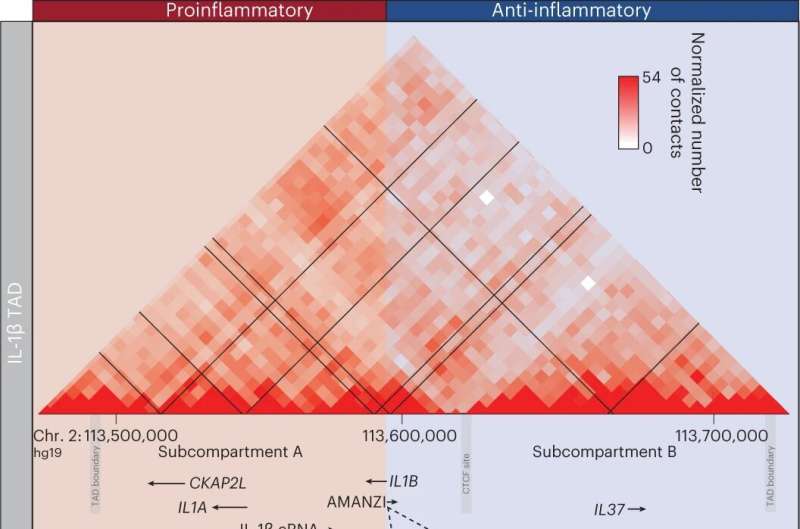
The researchers discovered that the SNP is part of a long stretch of non-coding RNA (lncRNA) they named AMANZI. AMANZI appears to be the director of interleukin-1β (IL-1β) which is at the core of the inflammatory process. After the BCG vaccine is administered, AMANZI activates IL-37 and triggers the anti-inflammatory response that regulates the activity of IL-1β.
This process of regulating IL-1β is important to achieving a long-term memory of vaccination through a process called trained immunity. Prof Mihai Netea at RUMC first observed trained immunity in 2013 to be important in how vaccines like BCG are protective.
"This process takes place in people with the G-SNP," says Mhlanga, "but it's less effective in people with an A-SNP. In the [A-SNP], AMANZI stably maintains the IL-37 'brake.' As a result, neither the immune responses to the vaccine nor the pathogen proceeds properly because IL-1β is dampened."
"So people with the G-SNP build up a functional defense, whereas in people with the A-SNP, this is not the case. To check, we removed the A-SNP AMANZI variant in white blood cells. As a result, we saw pro-inflammatory protection building up again, showing the effect of the one-letter difference in AMANZI once again."
Epigenetics
AMANZI exerts its influence by turning genes on and off in the research field of epigenetics. In the journal Nature Genetics, the researchers show in detail how long stretches of noncoding RNA (lncRNA) execute this and how small variations of just one letter affect such an epigenetic process, with profound consequences.
This applies not only to AMANZI but undoubtedly to many more lncRNAs, they argue. Those variations can be neutral but can also affect processes in the immune system negatively or positively.
In this particular case, it involves an interleukin-driven inflammatory process. Mhlanga says, "Several lncRNAs play a role in this process, and single-letter differences—SNP's, in other words—may also enhance or attenuate the effect of this inflammatory process. Further research is needed to understand the combined effect of multiple polymorphisms on these IL-1β-driven immune responses.
"Ultimately, we want to map all components of IL-1β signaling and trained immunity in order to find out their clinical usability. Importantly, nine out of ten SNPs are in noncoding regions of the genome."
More information: Ezio T. Fok et al, A chromatin-regulated biphasic circuit coordinates IL-1β-mediated inflammation, Nature Genetics (2023). DOI: 10.1038/s41588-023-01598-2


















