This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Japanese researchers warn that rates of urgent dialysis and death are on the rise
High blood pressure is called the silent killer because symptoms can remain hidden until a medical crisis strikes. You might think hypertension is no longer serious because blood pressure medication is widely available, but newly reported trends in people with dangerously high blood pressure might change your mind.
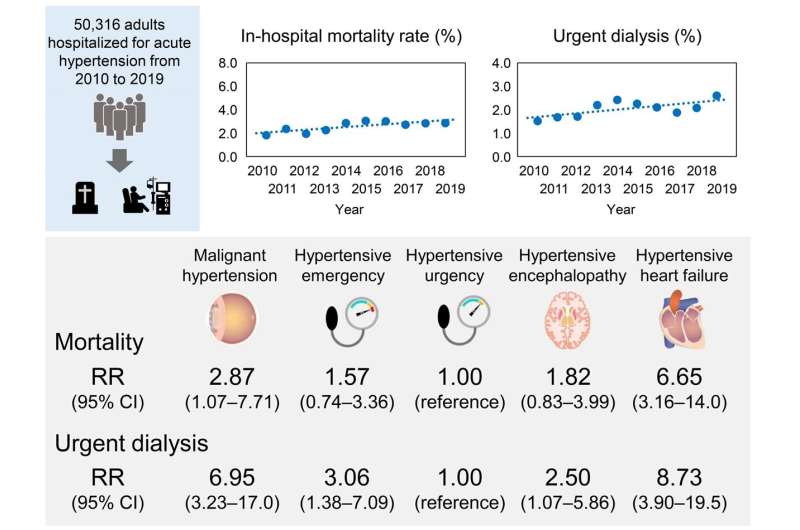
In a study recently published in Hypertension, researchers from Tokyo Medical and Dental University (TDMU) found that people admitted to the hospital over the last decade with spiking blood pressure—also known as acute hypertension—are increasingly likely to need urgent kidney dialysis or to die in the hospital.
The researchers examined the medical records of more than 50,000 patients admitted to the hospital for acute hypertension between 2010 and 2019. Over the study's ten years, urgent dialysis rates rose significantly, from 1.52% to 2.6%.
"Of note, the rising trend in urgent dialysis was similar in patients who were younger, male, or overweight, and those with hypertensive heart failure. People with these traits are a high-risk group," says the study's lead author, Hisazumi Matsuki. "Unfortunately, the urgent dialysis procedure can cause complications like infection or bleeding, which in turn may increase the patient's risk of dying."
Mortality rates also increased over the ten years from 1.83% to 2.88%, but not only because of the risks associated with urgent dialysis. "We saw a trend towards rising in-hospital mortality rates since 2010, particularly in patients who were elderly, male, and underweight, and in patients with hypertensive heart failure," says senior author Shintaro Mandai.
However, mortality rates were lower in patients who were overweight. "We observed the obesity paradox, which is an unexpected decrease in mortality that sometimes accompanies an increased body mass index," notes senior author Shinichi Uchida. "Underweight patients tend to have poor nutritional status and low physical activity and may have underlying conditions causing weight loss. Additionally, it can be difficult to find hidden heart congestion if the patient has no overt rise in blood pressure."
Despite advances in hypertension treatment, the authors note that there has been no decrease in the number of acute hypertension cases. High blood pressure leads to serious organ damage by altering the structure of blood vessels, which run through every part of the body. People with hypertension need appropriate outpatient care and intensive blood pressure control, such as blood pressure medication, exercise, and healthy diets.
The research also highlights the importance of detecting hidden congestion early and providing underweight patients with nutritional support. Measures must be taken to avoid as many unplanned hospital admissions due to acute hypertension as possible.
More information: Hisazumi Matsuki et al, National Trends in Mortality and Urgent Dialysis after Acute Hypertension in Japan From 2010 Through 2019, Hypertension (2023). DOI: 10.1161/HYPERTENSIONAHA.123.21880



















