This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Possible trigger of chronic inflammatory bowel disease identified
As the cause of chronic inflammatory bowel diseases (IBD) such as Crohn's disease or ulcerative colitis is not yet known, treatment for sufferers is currently aimed at alleviating the often agonizing symptoms. The discovery by a MedUni Vienna research team that the trigger for IBD could be found on the surface of intestinal epithelial cells provides a new potential starting point for the development of therapeutic measures.
The results of the study were recently published in the journal EMBO Reports.
In their experiments, the research group led by Bernadette Mödl and Robert Eferl from MedUni Vienna's Center for Cancer Research (CCR) and the Comprehensive Cancer Center (CCC) was able to show for the first time that certain changes in the brush border of intestinal epithelial cells could be associated with the development of IBD.
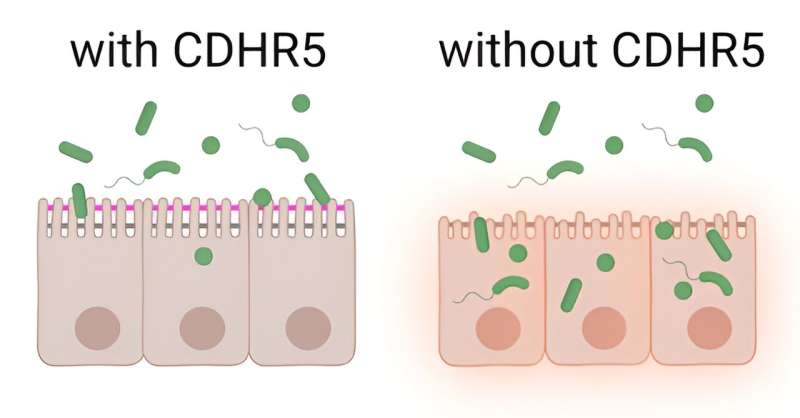
The brush border consists of dense, finger-shaped protrusions (microvilli) on the surface of the intestinal epithelial cells, the cells of the outermost layer of the intestine. The microvilli are connected to each other by a protein complex (intermicrovillar adhesion complex = IMAC), which is responsible for the organized structure of the brush border.
Boosting the production of certain proteins
It has been known for some time that a certain protein from the IMAC (CDHR5) is present in reduced amounts in people with IBD. In order to investigate the previously unknown connections, the research team created a mouse model for their investigations in which CDHR5 was missing. Electron microscopy revealed that the microvilli in the brush border of these mice appeared shortened and, like uncombed hair, completely disorganized.
"However, this alone did not lead to the invasion of harmful bacteria and the development of an intestinal infection," reports first author Bernadette Mödl. IBD only developed after the protective mucus layer over the intestinal epithelial cells was made permeable during the experiment.
"Reduced or missing IMAC protein and the associated organizational deficit in the brush border in combination with the permeability of the mucus layer have proven to be possible triggers of chronic inflammatory bowel diseases," says study leader Robert Eferl, summarizing the results.
Accordingly, active substances that boost the production of IMAC proteins in the intestinal epithelial cells could represent a possible starting point for the development of a causal therapy for IBD.
The fact that unhealthy, high-fat food is associated with the development of IBD can also be explained by the current study results, as this diet has been shown to make the mucus layer in the brush border of the intestinal epithelial cells more permeable. This could be particularly critical for people who have a family history of low CDHR5 production.
More information: Bernadette Mödl et al, Defects in microvillus crosslinking sensitize to colitis and inflammatory bowel disease, EMBO reports (2023). DOI: 10.15252/embr.202357084



















