This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Blood test could determine diabetes risks
A blood test could potentially be used to assess a patient's risk of type 2 diabetes, a new study from Edith Cowan University (ECU) has found.
The most commonly used inflammatory biomarker currently used to predict the risk of type 2 diabetes is high-sensitivity C-reactive protein (CRP). However, emerging research has suggested that the joint assessment of biomarkers, rather than assessing each individually, would improve the chances of predicting diabetes risk and diabetic complications.
A study by ECU researcher Dan Wu investigated the connection between systematic inflammation, assessed by joint cumulative high-sensitivity CRP and another biomarker called monocyte to high-density lipoprotein ratio (MHR), and incident type 2 diabetes.
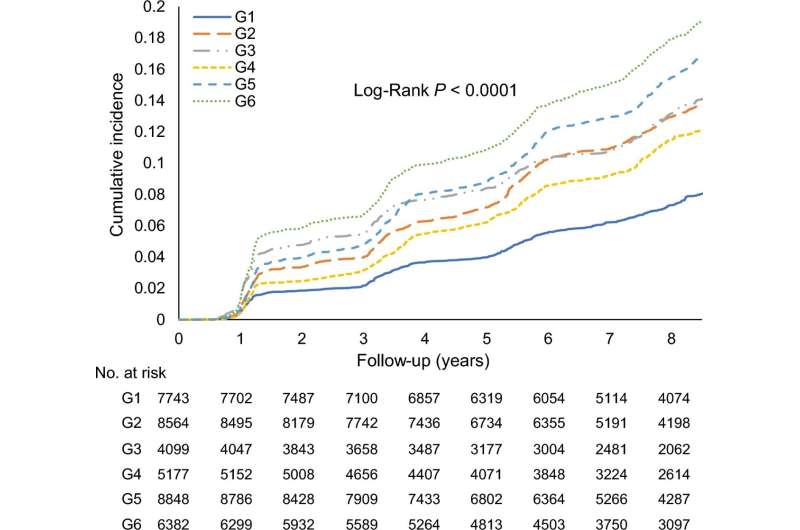
The study followed more than 40,800 non-diabetic participants over a nearly ten-year period, with more than 4,800 of the participants developing diabetes over this period. Wu said that of those patients presenting with type 2 diabetes, a significant interaction between MHR and CRP was observed.
"Specifically, increases in the MHR in each CRP stratum increased the risk of type 2 diabetes; concomitant increases in MHR and CRP presented significantly higher incidence rates and risks of diabetes."
"Furthermore, the association between chronic inflammation (reflected by the joint cumulative MHR and CRP exposure) and incident diabetes was highly age- and sex-specific and influenced by hypertension, high cholesterol, or prediabetes. The addition of the MHR and CRP to the clinical risk model significantly improved the prediction of incident diabetes," said Wu.
Females most at risk
The study found that females had a greater risk of type 2 diabetes conferred by joint increases in CRP and MHR, with Wu stating that sex hormones could account for these differences.
Wu said that the research findings corroborated the involvement of chronic inflammation in causing early-onset diabetes and merited specific attention.
"Epidemiological evidence indicates a consistent increase in early-onset diabetes, especially in developing countries. Leveraging this age-specific association between chronic inflammation and type 2 diabetes may be a promising method for achieving early identification of at-risk young adults and developing personalized interventions," she added.
Wu noted that the chronic progressive nature of diabetes and the enormous burden of subsequent comorbidities further highlighted the urgent need to address this critical health issue.
Although aging and genetics are non-modifiable risk factors, other risk factors could be modified through lifestyle changes. Inflammation is strongly influenced by life activities and metabolic conditions such as diet, sleep disruptions, chronic stress, and glucose and cholesterol dysregulation, thereby indicating the potential benefits of monitoring risk-related metabolic conditions.
Wu said that the dual advantages of cost-effectiveness and the wide availability of cumulative MHR and CRP in current clinical settings potentiated the widespread use of these measures as a convenient tool for predicting the risk of diabetes.
The study is published in the Journal of Translational Medicine.
More information: Dan Wu et al, Measurement of cumulative high-sensitivity C-reactive protein and monocyte to high-density lipoprotein ratio in the risk prediction of type 2 diabetes: a prospective cohort study, Journal of Translational Medicine (2024). DOI: 10.1186/s12967-024-04895-4



















