This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
A potential treatment for inflammatory bowel disease: Engineered yeast can transport medicines and lower inflammation
Inflammatory bowel disease (IBD) is a complex condition that requires individualized care to meet the needs of the patient's current disease state. With available medications sometimes causing serious side effects or losing their efficacy over time, many researchers have been exploring new, more targeted ways of delivering medications or other beneficial compounds, such as probiotics.
To address pitfalls in IBD treatment and drug delivery, the labs of Juliane Nguyen, Ph.D., professor and vice chair of pharmacoengineering and molecular pharmaceuticals at the UNC Eshelman School of Pharmacy, and Janelle Arthur, Ph.D., associate professor of microbiology and immunology at the UNC School of Medicine, have developed a genetically engineered probiotic strain of Saccharomyces boulardii.
In their new study published in Nature Communications, Nguyen, Arthur, and colleagues used mouse models to show that their engineered drug delivery system boosts probiotic concentrations and lengthens the probiotic yeast survival time in the gut. The improved probiotic uptake was also proven to inhibit and even reverse inflammation.
"We can now use this knowledge to better engineer probiotics to be more potent and to have more control over their function," said Nguyen, who is also a member of UNC Lineberger Comprehensive Cancer Center and the UNC McAllister Heart Institute. "Our long-term goal is to engineer an oral live biotherapeutic that can secrete specific therapeutics so that patients with IBD don't need to get painful injections or infusions with antibodies."
The human gut is a surprisingly harsh environment for oral probiotics due to its fortified microbiome. When new probiotics are introduced to the gut, it can be difficult for them to live and grow alongside well-established bacterial colonies. This challenge led Nguyen and Arthur to develop a live biotherapeutic delivery system that can survive and thrive in the gut.
For their targeted approach, researchers first needed to select a drug delivery vehicle for the study. They chose a yeast called Saccharomyces boulardii, which has been proven to be safe and well-tolerated in IBD patients, has anti-inflammatory properties, and can withstand antibiotic use.
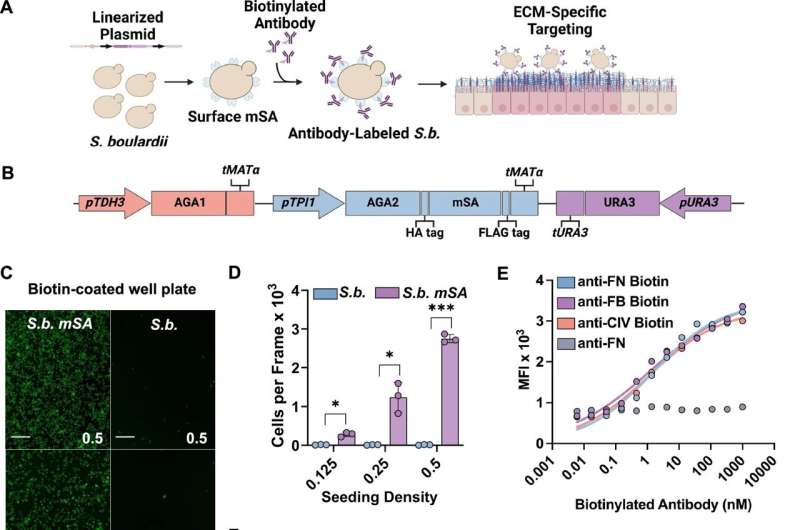
Mairead Heavey, Ph.D., who was the first author of the paper and a former Ph.D. candidate in Nguyen's lab, developed a platform surface display system. The method inserts surface proteins into the yeast's cell walls that are able to identify and target the proteins expressed by an IBD-affected colon.
The researchers specifically targeted proteins that are expressed by the extracellular matrix, the complex cellular network that is constantly being worn down by ulcers and rebuilding itself to form new intestinal tissue. When the extracellular matrix is working overtime to heal itself, it produces an increased number of proteins.
Using the upregulated proteins to their advantage, Nguyen and Arthur genetically altered the yeast with surface proteins that could target and bind to the extracellular matrix proteins for an extended period of time. With the system able to stick around for a while in the colon, the probiotic effects of the yeast will have enough time to kick in, providing some anti-inflammatory relief.
"What we are trying to do is endow this system with some capability to target ulceration and regions of increased extracellular matrix growth," said Arthur, who is also a member of UNC Lineberger Comprehensive Cancer Center. "We want to force it to stick around and colonize the gut, allowing it to have enough time to provide proper treatment and anti-inflammatory effects."
Over the course of 48 hours, researchers examined how well the surface display system stuck around in the colon. After 24–48 hours of probiotic gut residence time, there was a 100-fold increase in probiotic concentrations within the colon in preclinical models of ulcerative colitis, compared to their controls. As the probiotic gut residence time increased in the gut, researchers found that the colon length and inflammation improved and were eventually restored back to healthy levels.
Although the yeast has anti-inflammatory properties, it is not enough to provide relief for patients with IBD. Researchers engineered the yeast to produce antibodies and peptides that can target extracellular matrix proteins and provide treatment. Antibodies, which are a common anti-inflammatory treatment for IBD, can be switched out for other compounds that can be administered by the drug delivery system.
"We can easily exchange and pool compounds in the system," said Arthur. "Different compounds are needed depending on if a patient is having a flare-up or if they are in remission. We have the ability to swap out the compound actually to personalize it to the patient and their disease progression," added Nguyen.
Down the road, Nguyen and Arthur will examine how their system can be used to treat other gastrointestinal conditions, such as Clostridium difficile and colitis-associated colorectal cancer. Although their system is far from human clinical trials, the researchers are growing their team to include clinical experts who can help move their research from the laboratory to the clinic.
"I hope this work sparks further innovations in probiotic engineering," said Heavey. "I see so much potential as we continue to generate novel bioengineering methods and uncover the role of the microbiome in health and disease progression."
More information: Mairead K. Heavey et al, Targeted delivery of the probiotic Saccharomyces boulardii to the extracellular matrix enhances gut residence time and recovery in murine colitis, Nature Communications (2024). DOI: 10.1038/s41467-024-48128-0



















