This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Slowing inflammation may boost immunotherapy's effectiveness against advanced lung cancer
Adding an anti-inflammatory drug to anti-PD1 checkpoint inhibitor immunotherapy has shown great promise as a new strategy against advanced lung cancer, based on results from a small clinical trial led by investigators at the Abramson Family Cancer Center at the University of Pennsylvania Perelman School of Medicine.
The results published in Science, based the strategy on an accumulating body of evidence for the dual nature of inflammation—it can be beneficial against infectious pathogens and cancers in the short term, but can also lead to a weakened immune system when it becomes chronic. The paper is titled "Combined JAK Inhibition and PD-1 immunotherapy for non-small cell lung cancer patients."
Signs of this chronic inflammatory response, particularly involving a cytokine called interferon, are often seen in patients taking anticancer immunotherapies and are linked to worse outcomes.
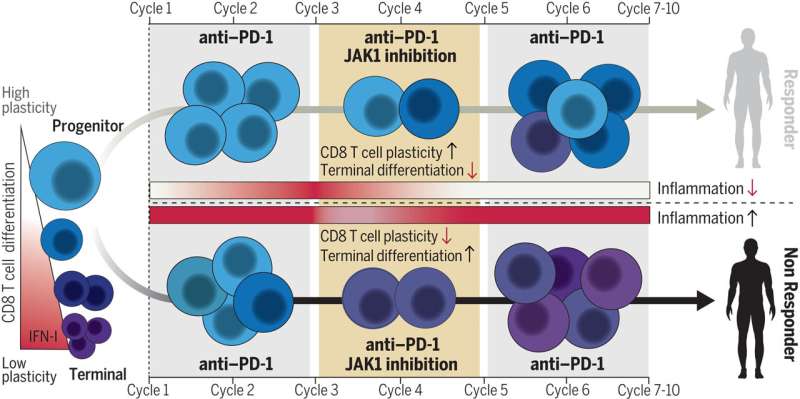
In the study, the researchers used a drug called a JAK1 inhibitor to specifically reduce persistent inflammatory signaling while not interfering with the initial inflammatory signaling required to generate antitumor activity. The JAK1 inhibitor was given for six weeks in 21 patients with advanced non-small cell lung cancer (NSCLC), but only after they had received two doses of anti-PD1 immunotherapy.
The result was an overall response rate of 67% and median progression-free survival of almost 24 months both of which are very high for advanced NSCLC.
"Many oncologists might find it surprising to combine a JAK inhibitor with immunotherapy since the focus has typically been on creating a strong inflammatory response for effective anti-PD1 treatment. However, there's a growing understanding that chronic inflammation, especially chronic interferon, can be harmful," said co-senior author Andy Minn, MD, Ph.D., professor of Radiation Oncology and director of the Mark Foundation Center for Immunotherapy, Immune Signaling, and Radiation.
"Our study's high response rate and the improvements in immune cells suggest that our approach could help control inflammation and interferon levels before they become detrimental."
"It's also encouraging that the best responders in this trial were those who had either low baseline inflammation or high baseline inflammation that responded to the JAK1 inhibitor treatment," said co-senior author E. John Wherry, MD, the Richard and Barbara Schiffrin President's Distinguished Professor, Chair of the Department of Systems Pharmacology & Translational Therapeutics, and Director of the Institute for Immunology and Immune Health.
The study's co-first authors were Divij Mathew, Ph.D., a postdoctoral researcher in the Wherry Lab, and Melina Marmarelis, MD, an assistant professor of Medicine (Hematology-Oncology) at the University of Pennsylvania Perelman School of Medicine and principal investigator of the clinical trial. Other study co-authors include Caitlin Foley, MD, Ph.D., a former medicine fellow in the Minn Lab, and Joshua Bauml, MD, former assistant professor of Medicine and co-principal investigator of the clinical trial.
Although the trial did not include a comparison group, the results suggested a striking effectiveness for the combination. The response rates for pembrolizumab alone in large clinical trials in stage 4 NSCLC patients usually has been approximately 45%. In this case, the overall response rate was 67%—and even now, a significant proportion of the patients remain alive, suggesting many of these responses are durable.
Analyses of the patients, and earlier tests in NSCLC mouse models, supported the treatment rationale: Lower levels of interferon-driven inflammation at baseline or following itacitinib treatment were associated with signs of a more effective CD8 T cell response—and better overall outcomes.
The researchers now plan to follow up with a larger confirmatory clinical trial as well as additional investigations into the role of JAK1 inhibition in patients with disease progression on immunotherapy, an area of great clinical need.
More information: Divij Mathew et al, Combined JAK inhibition and PD-1 immunotherapy for non–small cell lung cancer patients, Science (2024). DOI: 10.1126/science.adf1329



















