This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Revisiting effects of the pituitary-targeted gland axes on hepatic lipid homeostasis
Hepatic lipid homeostasis is critical for both cellular function and overall metabolic health. Disruptions in lipid homeostasis can lead to fatty liver diseases, which have become a significant global health concern. The evolving nomenclature and understanding of non-alcoholic fatty liver disease (NAFLD) have prompted renewed interest in its underlying mechanisms and broader metabolic implications. Central to these discussions is the role of the pituitary-targeted gland axes (PTGA) in regulating hepatic lipid metabolism.
The prevalence of NAFLD has increased alongside the rise in obesity and metabolic syndrome, making it the most common chronic liver disease worldwide. The proposed renaming of NAFLD to metabolic dysfunction-associated steatotic liver disease (MASLD) by various liver disease societies underscores the importance of metabolic factors in its pathogenesis.
Roles of hormones in hepatic lipid homeostasis
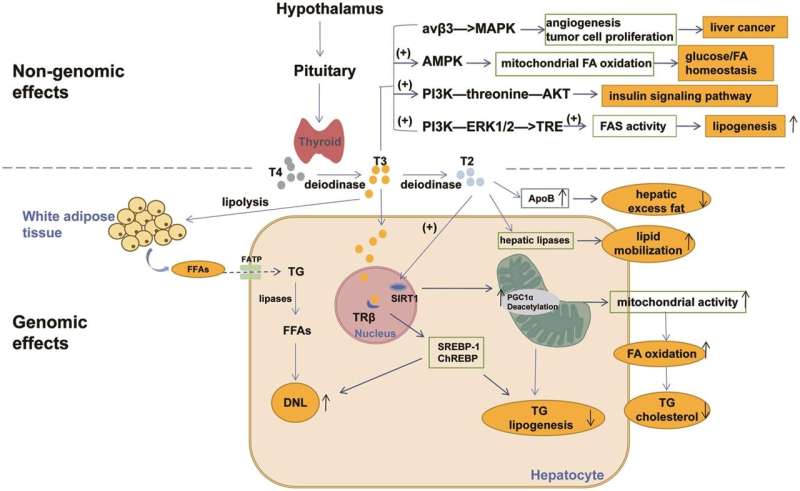
Thyroid hormones regulate metabolic rate and lipid metabolism. They influence the expression of genes involved in lipid synthesis, uptake, and degradation in the liver. Hypothyroidism is associated with reduced lipid breakdown and increased hepatic lipid accumulation, whereas hyperthyroidism can lead to decreased liver fat content. The balance of thyroid hormones is thus crucial for maintaining hepatic lipid homeostasis.
Adrenal hormones, particularly cortisol and catecholamines, significantly influence lipid metabolism. Cortisol promotes lipogenesis and inhibits lipid oxidation, which can induce hepatic steatosis. Chronic stress and adrenal dysfunction can exacerbate fatty liver conditions by altering these hormonal pathways. Additionally, catecholamines affect lipid mobilization from adipose tissue, further impacting liver fat content.
Estrogens and androgens play vital roles in liver fat metabolism. Estrogen deficiency, such as in postmenopausal women, is linked to increased hepatic lipid deposition. Conversely, excessive androgens, as seen in polycystic ovary syndrome (PCOS), also contribute to fatty liver disease. These hormones modulate lipid storage and mobilization, affecting overall liver health.
PTGA encompasses various endocrine glands whose hormones are regulated by pituitary signals. These hormones have far-reaching effects on metabolic processes, including hepatic lipid homeostasis. The pituitary gland influences thyroid, adrenal, and gonadal function, creating a network of feedback loops that ensure precise control over lipid metabolism. Disruptions in these axes, such as through pituitary tumors or systemic endocrine disorders, can lead to significant metabolic derangements, including fatty liver disease.
The therapeutic landscape for fatty liver diseases is expanding with the exploration of PTGA-related drugs. These pharmacological agents aim to modulate hormone levels or their receptors to restore lipid homeostasis. Examples include:
- Thyroid hormone analogs: These are designed to target hepatic pathways without causing systemic hyperthyroidism, thus improving liver function without adverse effects on other tissues.
- Selective glucocorticoid receptor modulators: These aim to mitigate the adverse metabolic effects of cortisol, reducing hepatic fat accumulation while preserving its essential functions.
- Hormone replacement therapies: Tailored to balance the beneficial effects of estrogen and androgens on lipid metabolism while minimizing potential risks, these therapies offer targeted interventions for hormonal imbalances contributing to fatty liver disease.
The concept of EAFLD underscores the interplay between endocrine disorders and fatty liver disease. Recognizing EAFLD emphasizes the need for a holistic approach to diagnosis and treatment, considering both hepatic and endocrine health.
This perspective is crucial for developing effective management strategies for patients with concurrent endocrine and liver disorders. By understanding the endocrine contributions to liver disease, clinicians can better address the multifaceted nature of these conditions and tailor treatments accordingly.
Understanding the roles of pituitary-targeted gland axes in hepatic lipid homeostasis opens new avenues for research and treatment of fatty liver diseases. Integrating endocrine health into the management of liver disease is essential for addressing the complexity of these conditions.
Future research should continue to explore PTGA-related mechanisms and therapies, advancing our knowledge and treatment options for hepatic lipid disorders. By recognizing and addressing the endocrine factors involved in fatty liver disease, we can improve patient outcomes and develop more effective therapeutic strategies.
The work is published in the Journal of Clinical and Translational Hepatology.
More information: Yifang Li et al, Effects of the Pituitary-targeted Gland Axes on Hepatic Lipid Homeostasis in Endocrine-associated Fatty Liver Disease-A Concept Worth Revisiting, Journal of Clinical and Translational Hepatology (2024). DOI: 10.14218/JCTH.2023.00421



















