This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Unlocking the secrets of the fibrotic fortress that surrounds and protects pancreatic cancer
While the overall five-year survival rate for pancreatic cancer is slowly improving, it remains discouragingly low—just 13%, according to the American Cancer Society. And the odds are even worse if the cancer is discovered after it has spread to other organs.
Mara Sherman, Ph.D., a cancer biologist at Memorial Sloan Kettering Cancer Center (MSK), is hoping to improve those grim statistics. Her lab is "all pancreas, all the time" and is focused primarily on illuminating interactions between cancer cells and the dense weave of fibrous cells that surrounds and protects pancreatic tumors. These fibers are like a layer of scar tissue that prevent drugs and immune defenders from reaching the cancer cells.
"We're particularly interested in the ecosystem that surrounds pancreatic tumors—what we call the tumor microenvironment—and how the noncancerous cells there impact how pancreatic cancer grows, spreads, and responds to therapy," says Dr. Sherman, a member of MSK's Sloan Kettering Institute, who moved to MSK from Oregon Health & Science University in early 2023.
These fiber-producing cells, or fibroblasts, make collagen and the extracellular matrix that gives shape and structure to our tissues. Fibroblasts can be found in many solid tumors, but they are remarkably abundant in pancreatic cancer. In healthy tissue, fibroblasts play a major role in wound healing, including releasing growth factors that help with tissue regeneration and the growth of blood vessels—characteristics that cancer cells happily exploit.
"Under the microscope, pancreas tumors look more like wounds than cancers, and two of the questions we're trying to understand are how much of this is specific to the pancreas, and how much of it is driven by pancreatic cancer cells?" she says.
What makes pancreatic cancer unique?
The location where cancer develops in the body matters. That's because cancer is not one disease, but many diseases—characterized by the abnormal growth of cells. Each type and subtype have their own characteristics, determined in part by the specific tissue where it developed.
Pancreatic cancer has two unique features, Dr. Sherman says.
First, almost all tumors in the pancreas develop due to mutations in the KRAS gene. (KRAS mutations were once considered "undruggable," but now KRAS inhibitors are starting to make a difference for patients whose tumors harbor these mutations.)
Second, the pancreas is home to a rare type of cell known as a stellate cell. These cells store vitamin A and help keep the tissue functioning properly. And in the context of inflammation and cancer, these cells change their behavior to become fibroblasts, driving the formation of dense fibers around the tumor.
"Not all of the cancer-associated fibroblasts in pancreatic cancer come from these stellate cells," Dr. Sherman says. "But we think there's something important about these cells that helps drive these tumors' ability to spread through metastasis. It's really early days, but we're starting to develop some new models to really dig into the why and how, in ways that we hope could pave the way for new therapeutic approaches."
Studying cancer's ecosystem
Dr. Sherman's lab is unique at MSK—and among a select number across the world—focusing on these fibrous cells associated with pancreatic cancer.
"Quite a few labs study pancreatic cancer and immune cells in the tumor microenvironment, but very little is known about these important noncancer, nonimmune cells," says Scott Lowe, Ph.D., who heads the Cancer Biology and Genetics Program at the Sloan Kettering Institute. "At MSK, we believe in studying cancer's entire ecosystem—which includes all the interactions between tumors and the tissues they inhabit, and the environment around different organs."
Interest in these fibroblasts is high, Sherman says, because of their abundance and prominence in pancreatic tumors. But the scientific tools and models for studying them are scarce compared to other key players like epithelial cells and immune cells.
"When you're working on these other cell types in the lab, investigators have beautifully specific mouse models and have other ways to genetically manipulate or fate-map cells of interest," she says. "For a number of reasons, fibroblasts are much harder to study, and we're basically in the position of having to develop new tools and methods."
Home-grown and publicly available datasets, however, along with new technologies like single-cell RNA sequencing are starting to peel back the layers of the onion.
"At MSK, we have some amazingly talented researchers who are experts in computational biology—so there's a lot of opportunity for collaboration," Dr. Sherman adds.
The effort to go beyond cancer genetics to focus on the greater context of cancer is consistent across the institution, which plans further research aimed at understanding cancer as a problem of malignant cells that are empowered or defeated by their host ecosystem.
A better way to study cells: Organoids
Another way the Sherman Lab is overcoming some of the limitations of traditional cell culture studies, where cells are grown in flat plastic dishes, is through the use of organoids. These millimeter-sized balls of cells are grown from tumor samples donated by patients, and they better mimic the properties and three-dimensionality of living tissue.
"When you grow these cancer-associated fibroblasts in a dish, they're all pretty much the same in terms of their form and their gene expression," Sherman says. "But when you grow them in an organoid, you really start to see a reemergence of the variation you see in human disease."
Identifying a new immune player in pancreatic cancer: Eosinophils
Fibroblasts aren't the only area of pancreatic cancer that the Sherman Lab is investigating.
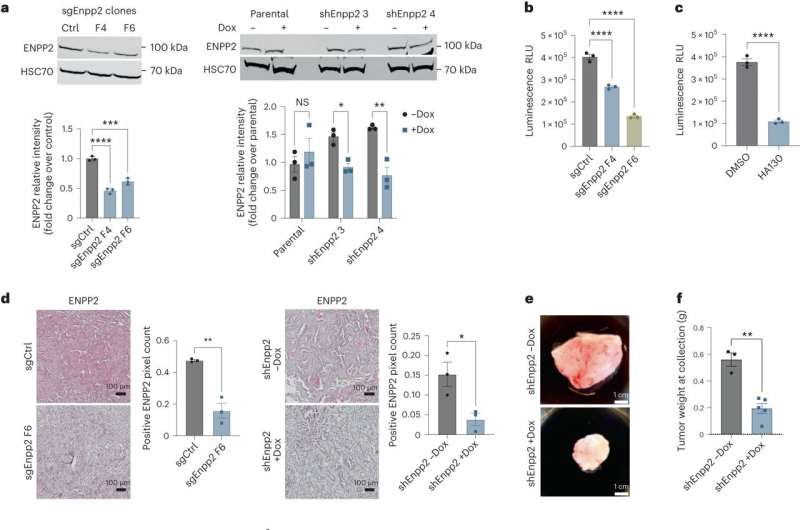
Earlier this year, Dr. Sherman's group published a study in Nature Cancer that shed new light on the role of a signaling molecule in the microenvironment around pancreatic tumors—one that holds potential for new treatment opportunities.
"We showed that this lysophosphatidic acid could act on pancreatic cancer cells and promote their proliferation," Dr. Sherman says. "But we suspected there was more to the story, given that this molecule lives in the extracellular space where it can also signal to other cell types besides cancer cells—like immune cells."
This signaling molecule was known to be involved in wound healing and in regulating the immune response in other types of cancer, and Dr. Sherman wanted to know how this process might influence the immune response in pancreatic cancer.
It turns out that a relatively rare type of white blood cell called an eosinophil was most affected by the signals. Yet eosinophils' role in pancreatic cancer had never been studied.
Sherman Lab research showed that an increase in the signaling molecule led to fewer eosinophils being recruited to the area around the tumor, and in turn, an increase in tumor cell proliferation.
"This project really picked up speed during the time of the pandemic when we were all homebound. This was also new territory for our lab," she says. "Postdoctoral fellow Sohinee Bhattacharyya, who led the research, connected with the International Eosinophil Society, and we were blown away by the generosity of this community of people who mostly study eosinophils in other diseases besides cancer."
Members of the group shared tools and techniques that helped the MSK team probe the role of eosinophils in pancreatic cancer.
Ultimately, the study showed that when this signaling lipid was reduced and more eosinophils were able to make it to the tumor, they helped limit its growth and check the cancer's ability to spread through metastasis.
The findings sparked hope that the discovery might help patients. In breast cancer, for example, more eosinophils have been associated with better responses to checkpoint inhibitor therapy, Dr. Sherman notes.
"We're encouraged that this may be a mechanism we could harness therapeutically to reduce the progression and spread of pancreatic cancer," she says. "And compounds that modulate this pathway are already starting to be explored in clinical trials."
The research will continue forward as Dr. Bhattacharyya completes her postdoctoral work at MSK and starts her own lab.
More information: Sohinee Bhattacharyya et al, Autotaxin–lysolipid signaling suppresses a CCL11–eosinophil axis to promote pancreatic cancer progression, Nature Cancer (2024). DOI: 10.1038/s43018-023-00703-y

















