This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Surprising mechanism of lupus kidney damage identified
A Berlin-led research team has uncovered critical regulators of severe kidney damage in patients with lupus, an autoimmune disorder affecting an estimated five million people worldwide, most of whom are young women. A small, specialized population of immune cells—called innate lymphoid cells (ILCs)—trigger an avalanche of effects that cause harmful kidney inflammation, also known as lupus nephritis.
The research, published this week in Nature, upends conventional wisdom that autoantibodies—proteins produced by immune cells that mistakenly attack healthy tissues—are primarily responsible for lupus nephritis.
"While autoantibodies are required for tissue damage, they are by themselves not sufficient. Our work reveals that ILCs are required to amplify the organ damage," says Dr. Masatoshi Kanda, a senior paper author who was a Humboldt Fellow at Max Delbrück Center and is now at the Department of Rheumatology and Clinical Immunology, Sapporo Medical University in Japan.
Lupus, or systemic lupus erythematosus, is most often diagnosed between the ages of 15 and 45. Symptoms can range from mild to severe. But what causes kidney damage in some patients—some to the point of requiring dialysis—has been unclear.
"The role of ILCs in lupus or lupus nephritis was entirely unknown," says Professor Antigoni Triantafyllopoulou, a senior paper author at the German Rheumatology Research Center (DRFZ), an institute of the Leibniz Association, and at the Department of Rheumatology and Clinical Immunology at Charité—Universitätsmedizin Berlin. "We have now identified most of the circuit controlled by ILCs by looking at the whole kidney at single-cell resolution."
Unusual immune cells
ILCs are a small group of immune cells that—unlike most other immune cells that circulate throughout the body—live in a specific tissue or organ.
"They are in the tissue all the time, from the time of embryonic development, which makes them very different from other immune cells," says Professor Andreas Diefenbach, a senior paper author and director of the Institute of Microbiology, Infectious Diseases and Immunology at Charité—Universitätsmedizin Berlin.
Diefenbach's lab was among those that discovered ILCs in the mid-2000s. Most of his research is focused on ILCs in the gut and how they modify tissue function. In this study, Triantafyllopoulou and Kanda teamed up with his group and Dr. Mir-Farzin Mashreghi at the DRFZ to find out whether ILCs were present in the kidney and what role they might play in lupus nephritis.
The whole single-cell picture
To unravel this mystery, the team turned to single-cell RNA sequencing, which identifies genes that are active, or "switched on," in individual cells and helps researchers understand the cell's identity and function.
Kanda, a rheumatologist who was studying bioinformatics in Professor Norbert Hübner's lab at the Max Delbrück Center at the time, developed a specialized protocol for single-cell RNA sequencing of mouse and human kidneys.
"Masatoshi's protocol was very good at pulling out and preserving multiple types of kidney cells, which gave us a much more complete overview of how lupus affects the whole kidney," explains Triantafyllopoulou. The team sequenced nearly 100,000 individual kidney and immune cells of various types and functions.
The key receptor
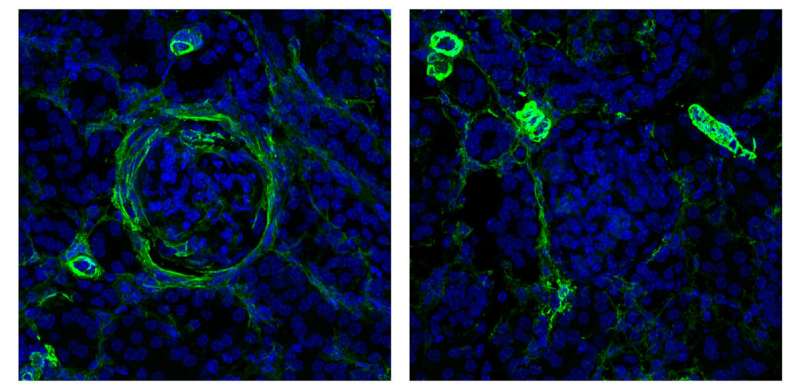
Through experiments in mice, the team learned that a subgroup of ILCs with a receptor called NKp46 must be present and activated to cause lupus nephritis. When NKp46 is activated, this subgroup of cells ramps up production of a protein called GM-CSF, which stimulates invading macrophages to multiply. Macrophages are large immune cells that gobble up dying cells and microbes. In the kidney, a flood of incoming macrophages causes severe tissue damage and buildup of scar tissue, called fibrosis.
"These ILCs are really amplifiers in this system," Diefenbach says. "They are small in population, but they seem to fertilize the whole process."
When the team blocked NKp46 with antibodies or the receptor was genetically removed, kidney tissue damage was minimal. They also blocked GM-CSF with similar anti-inflammatory effects.
"Critically, autoantibody levels did not change when NKp46 was inhibited, but kidney tissue damage was reduced, which shows autoantibodies are not directly responsible for kidney inflammation," Triantafyllopoulou explains.
The team also compared the results to sequencing data from tissue taken from human patients with lupus and found ILCs present, though more work is required to fully understand how to target ILCs in human kidneys. Nevertheless, the insights gained through these detailed studies point to new antibody therapies for patients with severe forms of lupus. The hope is to prevent the need for kidney dialysis in these patients.
More information: Stylianos-Iason Biniaris-Georgallis et al, Amplification of autoimmune organ damage by NKp46-activated ILC1, Nature (2024). DOI: 10.1038/s41586-024-07907-x





















