Researchers prevent mice from developing diabetes
(Medical Xpress) -- Swedish research group headed at Karolinska Institutet has been able to prevent onset of Type 1 diabetes in mice that are genetically susceptible to the disease. Through injection of specifically prepared cells, the researchers managed to stop the ongoing destruction of insulin-producing pancreatic beta cells in mice just prior to clinical debut of diabetes.
Type 1 diabetes is an autoimmune disease in which the immune system begins to attack and destroy the insulin-producing beta cells. This leads to a deficiency in production of insulin, which individuals with Type 1 diabetes thereafter have to inject. The initial cause of this autoimmune destruction is currently not known.
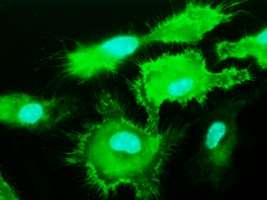
However, it is known that macrophages, a particular type of immune cells, have an active role in the destruction of pancreatic beta cells in Type 1 diabetes. Yet macrophages can also exhibit the opposite properties; earlier studies have demonstrated that macrophages can protect against inflammation-mediated tissue damage.
Immune cells utilise signal molecules termed cytokines in order to communicate with each other, giving instructions as to how the cells should act. In the current article, published in the scientific journal Diabetes, the researchers aimed to determine which cytokines were necessary to instruct macrophages to become protective cells.
"We managed to achieve this aim, defining a novel combination of cytokines that confer on macrophages the ability to protect mice from developing Type 1 diabetes", says Robert Harris, lead researcher at the Department of Clinical Neuroscience and based at the Centre for Molecular Medicine, Karolinska Institutet. "It has never previously been reported, that such an adoptive transfer cell therapy can be used in Type 1 diabetes and this study could thus represent a major advance towards disease prevention"
The researchers used so-called NOD mice which are genetically susceptible to developing Type 1 diabetes spontaneously between 12-30 weeks of age. The researchers grew macrophages from bone marrow progenitors from these mice. The mature macrophages were then stimulated with the defined combination of cytokines. When NOD mice were 16 weeks old separate groups were treated with either cytokine-stimulated macrophages, untreated macrophages of were not treated.
The mice were monitored for a further 12 weeks post-treatment. Using a specific three-dimensional imaging technique developed at Umeå University, Sweden, the degree of immune-mediated attack of the beta cells could be visualized in each treatment group. At the end of the follow-up period only 25% of the mice receiving the cytokine-treated macrophages had developed Type 1 diabetes, while 83% of the control groups had become sick.
"The cell therapy was initiated just 2 weeks before mice developed clinical diabetes", says Dr Harris. "At this stage few insulin-producing beta cells remain in the pancreas, yet we were able to protect these so that the mice never developed diabetes. Such a successful late-stage intervention has never previously been reported and is a significant result of our study. At the time of their clinical Type 1 diabetes diagnosis, most human individuals have already lost most of their insulin-producing beta cells."















