Pinning down the pain: Schwann cell protein plays major role in neuropathic pain
An international team of scientists, led by researchers at the University of California, San Diego School of Medicine, says a key protein in Schwann cells performs a critical, perhaps overarching, role in regulating the recovery of peripheral nerves after injury. The discovery has implications for improving the treatment of neuropathic pain, a complex and largely mysterious form of chronic pain that afflicts over 100 million Americans.
The findings are published in the March 27, 2013 issue of the Journal of Neuroscience.
Neuropathic pain occurs when peripheral nerve fibers (those outside of the brain and spinal cord) are damaged or dysfunctional, resulting in incorrect signals sent to the brain. Perceived pain sensations are frequently likened to ongoing burning, coldness or "pins and needles." The phenomenon also involves changes to nerve function at both the injury site and surrounding tissues.
Not surprisingly, much of the effort to explain the causes and mechanisms of neuropathic pain has focused upon peripheral nerve cells themselves. The new study by principal investigator Wendy Campana, PhD, associate professor in UC San Diego's Department of Anesthesiology, with colleagues at UC San Diego and in Japan, Italy and New York, points to a surprisingly critical role for Schwann cells – a type of glial support cell.
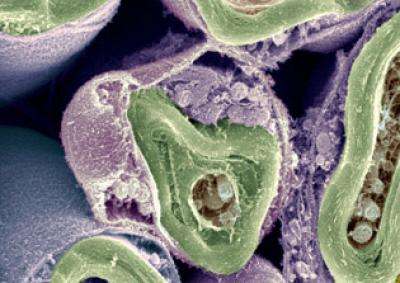
Schwann cells promote the growth and survival of neurons by releasing molecules called trophic factors, and by supplying the myelin used to sheathe neuronal axons. Myelination of axons helps increase the speed and efficacy of neural impulses, much as plastic insulation does with electrical wiring.
"When Schwann cells are deficient they can't perform these functions," said Campana. "Impaired neurons remain impaired and acute damage may transition to become chronic damage, which can mean lasting neuropathic pain for which there is currently no effective treatment."
Specifically, the scientists investigated a protein called LRP1, which Campana and colleagues had first identified in 2008 as a potential basis for new pain-relieving drugs due to its signal-blocking, anti-inflammatory effects.
The researchers found that mice genetically engineered to lack the gene that produces LRP1 in Schwann cells suffered from abnormalities in axon myelination and in Remak bundles – multiple non-myelinated pain transmitting axons grouped together by Schwann cells. In both cases, one result was neuropathic pain, even in the absence of an actual injury.
Moreover, injured mice lacking the LRP1 gene showed accelerated cell death and poor neural repair compared to controls, again resulting in significantly increased and sustained neuropathic pain and loss of motor function.
"LRP1 helps mediate normal interactions between Schwann cells and axons and, when peripheral nerves have been injured, plays a critical role in regulating the steps that lead to eventual nerve regeneration," said Campana. "When LRP1 is deficient, defects and problems become worse. They may go from acute to chronic, with increasing levels of pain."
Campana and others are now pursuing development of a small molecule drug that can mimic LRP1, binding to receptors in Schwann cells to improve their health and ability to repair damaged nerve cells. "By targeting Schwann cells and LRP1, I think we can improve cells' response to injury, including reducing or eliminating chronic neuropathic pain."



















