Scientists map molecular mechanism that may cause toxic protein buildup in dementing disorders
There is no easy way to study diseases of the brain. Extracting brain cells, or neurons, from a living patient is difficult and risky, while examining a patient's brain post-mortem usually only reveals the disease's final stages. And animal models, while incredibly informative, have frequently fallen short during the crucial drug-development stage of research. But scientists at the Gladstone Institutes and the University of California, San Francisco (UCSF) have taken a potentially more powerful approach: an advanced stem-cell technique that creates a human model of degenerative disease in a dish.
Using this model, the team uncovered a molecular process that causes neurons to degenerate, a hallmark sign of conditions such as Alzheimer's disease and frontotemporal dementia (FTD). The results, published in the latest issue of Stem Cell Reports, offer fresh ammunition in the continued battle against these and other deadly neurodegenerative disorders.
The research team, led by Gladstone Investigator Yadong Huang, MD, PhD, identified an important mechanism behind tauopathies. A group of disorders that includes both Alzheimer's and FTD, tauopathies are characterized by the abnormal accumulation of the protein Tau in neurons. This buildup is thought to contribute to the degeneration of these neurons over time, leading to debilitating symptoms such as dementia and memory loss. But while this notion has been around for a long time, the underlying processes have largely remained unclear.
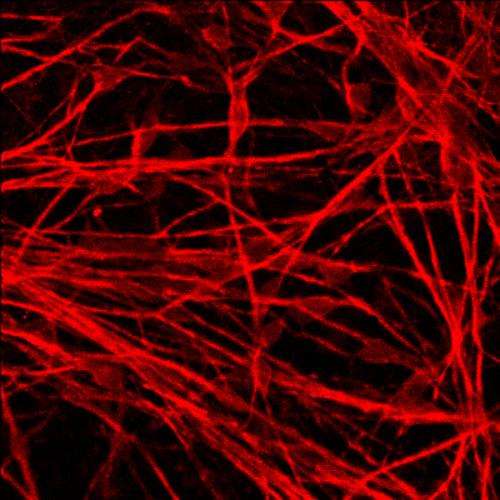
"So much about the mechanisms that cause tauopathies is a mystery, in part because traditional approaches—such as post-mortem brain analysis and animal models—give an incomplete picture," explained Dr. Huang, who is also an associate professor of neurology at UCSF, with which Gladstone is affiliated. "But by using the latest stem-cell technology, we generated human neurons in a dish that exhibited the same pattern of cell degeneration and death that occurs inside a patient's brain. Studying these models allowed us to see for the first time how a specific genetic mutation may kick start the tauopathy process."
Other scientists recently discovered that the Tau mutation in question could increase a person's risk of developing different tauopathies, including Alzheimer's or FTD. So the research team, in collaboration with Bruce Miller, MD, who directs the UCSF Memory and Aging Center and who provided skin cells from a patient with this mutation, transformed these cells into induced pluripotent stem cells, or iPS cells. This technique, pioneered by Gladstone Investigator and 2012 Nobel Laureate Shinya Yamanaka, MD, PhD, allows scientists to reprogram adult skin cells into cells that are virtually identical to stem cells. These stem cells can then develop into almost any cell in the body.
The team combined this method with a cutting-edge gene-editing technique that essentially eliminated the Tau mutation in some of the iPS cells. The result was a system that allowed the team to compare neurons that had the mutation to those that did not.
"Our approach allowed us to grow human neurons in a dish that contained the exact same mutation as the neurons in the brain of the patient," explained first author Helen Fong, PhD, who is also a California Institute for Regenerative Medicine postdoctoral scholar. "By comparing these diseased neurons with the 'genetically corrected' healthy neurons, we could see—cell by cell—how the Tau mutation leads to the abnormal build up of Tau and, over time, neuronal degeneration and death."
"Tau's main functions include keeping the skeletal structure of individual neurons intact and regulating neuronal activity," said Dr. Huang. "But our research showed that the Tau produced by neurons from people with the Tau mutation is different; so it is red-flagged by the cell and targeted for destruction. However, instead of being flushed out, Tau gets chopped into pieces. These potentially toxic fragments accumulate over time and may in fact cause the neuron to degenerate and die."
But by correcting the Tau mutation, the team effectively removed Tau's red flag. The protein remained in one piece, the abnormal buildup ceased and the neurons remained healthy. Ongoing studies aim to determine whether the abnormal fragmentation of mutant tau is really the main cause of the neuronal death and, if so, how to block it.
"These findings not only offer a glimpse into how these powerful new models can shed light on disease mechanisms" said Dr. Miller, "They may also prove invaluable for screening potential drugs that could be developed into better treatments for Alzheimer's disease, FTD, and related conditions."
















