Unique protein interaction may drive most common genetic cause of Parkinson's disease
The most devastating aspect of Parkinson's disease may not be its debilitating symptoms, which rob its victims of their ability to control their own movement. It may not be the millions around the world and their families who suffer each day from the disease's harmful effects. Instead, it may in fact be that its root causes remain largely a mystery. But now, scientists at the Gladstone Institutes have discovered how the interplay between two proteins in the brain fuels the degradation and death of the class of brain cells, or neurons, that leads to Parkinson's. These findings, which stand in stark contrast to conventional wisdom, lay much-needed groundwork for developing treatments that target the disease's elusive underlying mechanisms.
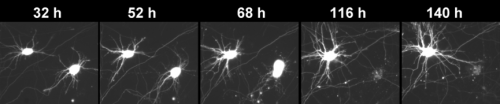
In the latest issue of the Journal of Neuroscience, now available online, scientists in the laboratory of Gladstone Investigator Steve Finkbeiner, MD, PhD, harnessed the power of their one-of-a-kind robotic microscope to track the lifespan of individual neurons over time. The microscope has been used to study a variety of neurodegenerative diseases, and in this study, they focus their attention on LRRK2—the most common genetic cause of Parkinson's.
Scientists have long known that mutations in LRRK2 cause misfolded versions of the LRRK2 protein to accumulate in neurons. The prevailing hypothesis has been that misfolded LRRK2 boosts the activity of a type of enzyme called kinase, and that this heightened kinase activity is what drives cell death. Scientists have also looked to the fact that mutant LRRK2 tends to clump together into so-called inclusion bodies (IB's) as another contributor to the disease's progression.
"As a result, researchers have used the presence of IB's and heightened kinase activity as a proxy for measuring LRRK2's harmful effects, rather than measuring LRRK2 levels directly," explained Dr. Finkbeiner, who is the associate director of neurological research at Gladstone as well as a professor at the University of California, San Francisco, with which Gladstone is affiliated. "But we were unconvinced that these were the main drivers of cell death—so we decided to take a closer look at what was happening inside the cell."
When studying neurodegenerative diseases such as Parkinson's, which are defined by the degradation and death of neurons, traditional tools usually only allow researchers to track neuronal death at the population level. But Dr. Finkbeiner's revolutionary microscope enables researchers to follow the lives of thousands of individual neurons—offering the clearest view into which events during the lifetime of the cell play a role in its death.
The researchers generated neurons from two sources: from rats genetically modified to have mutant LRRK2, and human neurons derived from the skin cells of LRRK2-related Parkinson's patients. They then tracked these cells over time, monitoring the buildup of mutant LRRK2 and how that buildup led to cell death.
"Interestingly, we found that neither IB's nor kinase activity were the direct cause of cellular toxicity leading to neuronal death,," said Gladstone Staff Research Scientist Gaia Skibinski, PhD, the paper's lead author. "Instead, the underlying cause of cell death appeared to be tied directly to the accumulation of diffuse mutant LRRK2."
But as the research team peered even closer into the lives of these neurons, they found something intriguing: a unique interplay between mutant LRRK2 and alpha-synuclein, another protein that has long been associated with Parkinson's. Research has shown that Parkinson's patients with LRRK2 mutations often show an abnormal accumulation of alpha-synuclein. But until now, the exact nature of the relationship between these two proteins remained unclear.
"Importantly, we found that in both the rat and human cellular models, removing alpha-synuclein reduced cell death caused by mutant LRRK2," continued Dr. Skibinski. "When we looked closer, we found that loss of alpha-synuclein led to an immediate drop in LRRK2."
The team hypothesizes that, in patients with mutant LRRK2, the build-up of alpha-synuclein hinders the cell's ability to clear away LRRK2, leading to its accumulation. Over time, the buildup of LRRK2 becomes toxic to the cell, and the cell dies.
"The discovery of a synergistic relationship between two proteins long known to play a role in Parkinson's is a huge step towards developing drugs that attack the disease's underlying mechanisms," said Dr. Finkbeiner. "As we continue to unravel the precise functional relationship between alpha-synuclein and LRRK2, we are well on our way to halting the onslaught of Parkinson's on the brain."
















