Study urges caution in stem cell clinical trials for heart attack patients
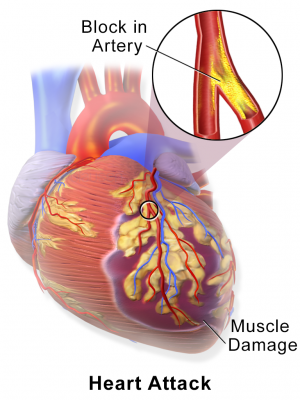
A new study in Nature challenges research data that form the scientific basis of clinical trials in which heart attack patients are injected with stem cells to try and regenerate damaged heart tissue.
Researchers at Cincinnati Children's Hospital Medical Center and the Howard Hughes Medical Institute (HHMI), report May 7 that cardiac stem cells used in ongoing clinical trials – which express a protein marker called c-kit – do not regenerate contractile heart muscle cells at high enough rates to justify their use for treatment.
Including collaboration from researchers at Cedars-Sinai Heart Institute in Los Angeles and the University of Minnesota's Lillehei Heart Institute, the study uncovers new evidence in what has become a contentious debate in the field of cardiac regeneration, according to Jeffery Molkentin, PhD, study principal investigator and a cardiovascular molecular biologist and HHMI investigator at the Cincinnati Children's Heart Institute.
"Our data suggest any potential benefit from injecting c-kit-positive cells into the hearts of patients is not because they generate new contractile cells called cardiomyocytes," Molkentin said. "Caution is warranted in further clinical testing of this method until the mechanisms in play here are better defined or we are able to dramatically enhance the potential of these cells to generate cardiomyocytes."
Numerous heart attack patients have already been treated with c-kit-positive stem cells that are removed from healthy regions of a damaged heart then processed in a laboratory, Molkentin explained. After processing, the cells are then injected into these patients' hearts. The experimental treatment is based largely on preclinical studies in rats and mice suggesting that c-kit-positive stem cells completely regenerate myocardial cells and heart muscle. Thousands of patients have also previously undergone a similar procedure for their hearts but with bone marrow stem cells.
Molkentin and his colleagues report those previous preclinical studies in rodents do not reflect what really occurs within the heart after injury, where internal regenerative capacity is almost non-existent. Molkentin also said that combined data from multiple clinical trials testing this type of treatment show most patients experienced a roughly 3-5 percent improvement in heart ejection fraction – a measurement of how forcefully the heart pumps blood. Data in the current Nature study suggest this small benefit may come from the ability of c-kit-positive stem cells in heart to cause the growth of capillaries, which improves circulation within the organ, but not by generating new cardiomyocytes.
"What we show in our study is that c-kit-positive stem cells from the heart like to make endothelial cells that form capillaries. But in their natural environment in the heart, these c-kit positive cells do not like to make cardiomyocytes," Molkentin said. "They will produce cardiomyocytes, but at rates so low – roughly one in every 3,000 cells – it becomes meaningless."
The c-kit protein is expressed on the surface of progenitor cells originally identified in bone marrow. These c-kit expressing cells can generate multiple different cell types that are destined to help form specific organ tissues or other parts of the body. Given its presence in bone marrow, c-kit cells are also involved in the production of different types of immune system cells.
Researchers in the current study worked with two lines of genetically bred mice to see how efficiently c-kit-positive cardiac progenitor cells would regenerate cardiomyocytes in the hearts of the animals. The authors measured heart cell regeneration rates during the animals' embryonic development, during aging and after myocardial infarction (heart attack).
The mice were bred so that a fluorescent protein marker was permanently added to any cell that expressed the Kit gene, regardless of what it then turned into. This allowed the scientists to track the specific types and volumes of any c-kit-positive cells being generated in the animals, including in their hearts.
Test results showed that c-kit-positive cells originating in the heart generated new cardiomyocytes at a percentage (from baseline) of 0.03 or less. The authors go on to report that the percentage of new cardiomyocyte generation actually falls to below 0.008 when considering a natural process called cellular fusion – which in this instance involves c-kit-positive cells from the bone marrow or circulating immune system cells fusing with cardiomyocytes in the heart.
As a follow up to the current study, Molkentin and his colleagues are currently testing genes and protein growth factors that may be able to boost the rate of new cardiomyocyte generation from c-kit-positive stem cells. Because the current study shows that endogenous c-kit cells at least have some limited ability to regenerate contractile heart cells, Molkentin said it may be possible to find a method to enhance this ability genetically so the cells can eventually be used in a truly therapeutically beneficial manner to make new contractile activity in the heart.
More information: Paper: c-kit+ cells minimally contribute cardiomyocytes to the heart, dx.doi.org/10.1038/nature13309

















