Engineered stem cells seek out, kill HIV in living organisms
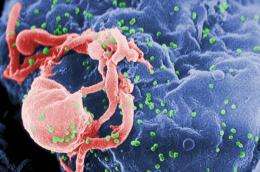
(Medical Xpress) -- Expanding on previous research providing proof-of-principal that human stem cells can be genetically engineered into HIV-fighting cells, a team of UCLA researchers have now demonstrated that these cells can actually attack HIV-infected cells in a living organism.
The study, published April 12 in the journal PLoS Pathogens, demonstrates for the first time that engineering stem cells to form immune cells that target HIV is effective in suppressing the virus in living tissues in an animal model, said lead investigator Scott G. Kitchen, an assistant professor of medicine in the division of hematology and oncology at the David Geffen School of Medicine at UCLA and a member of the UCLA AIDS Institute.
"We believe that this study lays the groundwork for the potential use of this type of an approach in combating HIV infection in infected individuals, in hopes of eradicating the virus from the body," he said.
In the previous research, the scientists took CD8 cytotoxic T lymphocytes — the "killer" T cells that help fight infection — from an HIV-infected individual and identified the molecule known as the T cell receptor, which guides the T cell in recognizing and killing HIV-infected cells. However, these T cells, while able to destroy HIV-infected cells, do not exist in great enough quantities to clear the virus from the body. So the researchers cloned the receptor and used this to genetically engineer human blood stem cells. They then placed the engineered stem cells into human thymus tissue that had been implanted in mice, allowing them to study the reaction in a living organism.
The engineered stem cells developed into a large population of mature, multi-functional HIV-specific CD8 cells that could specifically target cells containing HIV proteins. The researchers also discovered that HIV-specific T cell receptors have to be matched to an individual in much the same way an organ is matched to a transplant patient.
In this current study, the researchers similarly engineered human blood stem cells and found that they can form mature T cells that can attack HIV in tissues where the virus resides and replicates. They did so by using a surrogate model, the humanized mouse, in which HIV infection closely resembles the disease and its progression in humans.
In a series of tests on the mice's peripheral blood, plasma and organs conducted two weeks and six weeks after introducing the engineered cells, the researchers found that the number of CD4 "helper" T cells — which become depleted as a result of HIV infection — increased, while levels of HIV in the blood decreased. CD4 cells are white blood cells that are an important component of the immune system, helping to fight off infections. These results indicated that the engineered cells were capable of developing and migrating to the organs to fight infection there.
The researchers did note a potential weakness with the study: Human immune cells reconstituted at a lower level in the humanized mice than they would in humans, and as a result, the mice's immune systems were mostly, though not completely, reconstructed. Because of this, HIV may be slower to mutate in the mice than in human hosts. So the use of multiple, engineered T cell receptors may be one way to adjust for the higher potential for HIV mutation in humans.
"We believe that this is the first step in developing a more aggressive approach in correcting the defects in the human T cell responses that allow HIV to persist in infected people," Kitchen said.
The researchers will now begin making T cell receptors that target different parts of HIV and that could be used in more genetically matched individuals, he said.
More information: Research paper online: dx.plos.org/10.1371/journal.plpa.1002649















