Human diabetes has new research tool: Overfed fruit flies that develop insulin resistance
(Medical Xpress) -- With Type 2 human diabetes climbing at alarming rates in the United States, researchers are seeking treatments for the disease, which has been linked to obesity and poor diet.
Now biologists at Southern Methodist University, Dallas, report they have developed a new tool that will help researchers better understand this deadly disease.
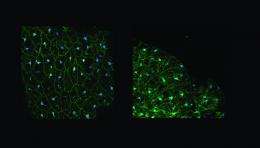
By manipulating the diets of healthy adult fruit flies, the researchers developed flies that are insulin-resistant, a hallmark of Type 2 diabetes.
Until now, researchers largely have relied on rats, mice and other animals as model systems for exploring the metabolic and genetic changes that take place in diabetics.
The fruit fly Drosophila melanogaster has been widely deployed in labs to investigate a wide range of human diseases, from Alzheimer’s to cancer. But the scientific literature hasn’t documented use of the adult fruit fly for studying the metabolic disruptions that are the hallmark of Type 2 diabetes. The fruit fly’s advantages include its low cost and a very short lifespan, both of which enable scientists to undertake rapid screenings in their search for new genetic and drug treatments.
The insulin-resistant fruit fly was developed in the lab of SMU biologist Johannes H. Bauer, principal investigator for the study. It was accomplished by feeding fruit flies a diet high in nutrients, said Bauer, an assistant professor in SMU’s Department of Biological Sciences. That process mimics one of the ways insulin resistance develops in humans — overeating to the point of obesity.
The lab’s insulin-resistant fruit flies now can serve as a highly relevant and efficient model for studying Type 2 diabetes.
“We learned that by manipulating the nutrients of fruit flies, we can make them insulin resistant,” Bauer said. “With this insulin-resistant model we can now go in with pinpoint precision and study the molecular mechanisms of insulin resistance, as well as drug treatments for the condition, as well as how to treat obesity, how to block insulin resistance and how metabolic changes from a specific diet develop. The possibilities are endless.”
The researchers reported their findings in the article “Development of diet-induced insulin resistance in adult Drosophila melanogaster,” published in Biochimica et Biophysica Acta – Molecular Basis of Disease.
Two overfeeding diets, carb and protein, both result in insulin resistance
Insulin, produced by the pancreas, is the hormone that tells our cells to absorb glucose, a necessary sugar molecule that provides our body, particularly the brain, with the energy to function, make repairs, move and grow.
In Type 2 diabetes, a person is insulin-resistant because his or her cells fail to respond to insulin’s signal to absorb glucose. The disregulation of glucose upsets the body’s delicate internal equilibrium, causing massive disruptions in normal cellular processes. These interruptions manifest in multiple disease symptoms, making Type 2 diabetes difficult to characterize, treat and cure.
To provide a good base model organism to study aspects of this complex disease, researchers in the Bauer lab wanted to determine whether flies develop diabetes-like metabolic changes when fed different diets. The researchers developed the insulin-resistant flies in two different ways: One group of fruit flies was overfed a carbohydrate-loaded diet; a second group of flies was overfed a protein-loaded diet. In both cases, the disruption had a profoundly detrimental effect on the flies’ health and physiology.
SMU biologist Siti Nur Sarah Morris, lead author on the study, said the results the researchers observed were both expected and unexpected. The researchers expected the flies to gain weight, which they did. Carb-loaded flies gained excessive weight and got fat, just like humans who overeat sweets, french fries, pasta and ice cream. Protein-loaded flies also gained weight, but upon extreme overfeeding they lost weight, just like humans who follow the popular Atkins Diet, a weight loss program in which participants eat only meat, seafood and eggs.
The researchers expected the carb-loaded fruit flies to develop insulin resistance, which they did.
In a surprising result, however, the fruit flies that overate protein also developed insulin resistance, but at a quicker and more severe rate.
“Carb-loaded flies gain weight. Protein-loaded flies gain and then lose weight. So the two diets have exactly opposite effects on metabolism,” Bauer said. “But too much of either one of them causes insulin resistance. That surprised us.”
Overfed flies had shortened lifespans, differences in fertility
In other findings, carb-loaded flies experienced a profound decline in egg-laying, a measurement of fertility. In contrast, protein-loaded flies first experienced increased egg-laying, but the extreme diet led to decreased egg laying. Both diets led to shortened longevity, the scientists reported.
“The high-protein flies looked frail and unhealthy. They moved less, almost as if sedated,” Morris said. “The fatter flies on the high-carb diet had massively decreased fertility; they flew less but still tried to move.”
While both diets resulted in insulin resistance, differences were remarkable.
“The carb data imply a linear relationship between carb levels and health. The more carbs, the more weight, the more sugar storage and fat, the more insulin resistance and the less fertility,” Bauer said. “But with protein, this relationship becomes parabolic, meaning all readouts go up, then come down again. The decreased storage we liken to a catabolic state that is primarily destructive for the body’s optimum metabolic functioning, such as the ketosis typically seen in people eating Atkins-type diets.”
Besides Morris and Bauer, other authors on the study were SMU students Claire Coogan, Khalil Chamseddin and Santharam Kolli. Other co-authors, from Pennington Biomedical Research Center, Baton Rouge, La., are Jeffrey N. Keller, director, Institute of Dementia Research & Prevention, and Sun Ok Fernandez-Kim. The research was funded by the National Institute on Aging.

















