Rice researcher rebooting 'deep brain stimulation'
Deep brain stimulators, devices that zap Parkinson's disease tremors by sending electrical current deep into nerve centers near the brain stem, may sound like they are cutting-edge, but Rice University's Caleb Kemere wants to give them a high-tech overhaul.
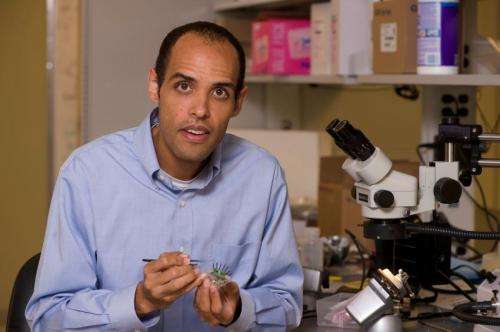
Kemere, who's equal parts electrical engineer and neuroscientist, specializes in building electronic devices that interact with the brain. One longtime area of interest is the basal ganglia, the part of the brain that helps govern movement; it's also the nerve center targeted by "deep brain stimulation" (DBS) technology, a neuroelectronic device that's sometimes used to treat patients in the late stages of Parkinson's.
Thanks to a new five-year grant from the National Science Foundation (NSF), Kemere is about to embark on a program to reboot DBS technology with the latest embedded processors and research analytics. The research is funded by an NSF CAREER Award. The NSF gives only about 400 CAREER Awards each year across all disciplines. The program is designed to support the research and career development for young scholars that the agency expects to become leaders in their field. Each award includes about $400,000 in research funding.
"Deep brain stimulation has proven to be remarkably effective in treating Parkinson's, and it may well turn out to be revolutionary for treating severe depression and other neurological and psychiatric disorders," said Kemere, assistant professor of electrical and computer engineering and director of Rice's Realtime Neural Engineering Laboratory.
DBS systems, which are sometimes called "brain pacemakers," deliver a small, continuous current to the basal ganglia of late-stage Parkinson's patients. The technology can produce dramatic results and it allows some Parkinson's patients to walk, speak, write and perform other motor movements that are exceedingly challenging when the device is switched off.
"Today's DBS technology is basically the same as that used in heart pacemakers," Kemere said. "The electrodes are just implanted inside the brain rather than in the heart. I've found that when electrical engineers like myself first hear about DBS, they generally have the same two thoughts: 'Wow, that's a really cool use of electronics,' and 'The brain doesn't pulse like a heart; maybe we can improve this by matching the stimulation to the dynamic nature of the brain!'
"It's that second idea that we're focused on here," said Kemere, who is also an adjunct assistant professor of neurology at Baylor College of Medicine. "We want to develop deep brain stimulation technology that operates on the order of milliseconds, actively detecting what's going on in the brain at any moment and then modulating the stimulation to optimize results. In electrical engineering terms, we call this 'closing the feedback loop.'"
Kemere said today's DBS systems are manually adjusted by neurologists when a patient comes in for an office visit every few weeks or months. In his next-generation DBS, these types of adjustments would be made automatically, many times each second.
"There are several reasons we want to do this," Kemere said. "Though DBS is remarkably effective today, it provides only minimal therapeutic benefit for perhaps a third of Parkinson's patients. It's possible that dynamic DBS could substantially increase effectiveness for these users.
"Also, current DBS technology has side effects, and we'd like to reduce those," Kemere said. "For example, people with Parkinson's have a spectrum of symptoms, including tremors, trouble initiating muscle movement, muscle rigidity and slowness of movement. Sometimes, DBS can relieve one of those symptoms but make another one worse."
Rebooting DBS technology won't be simple. For starters, the real-time computer processing required for dynamic DBS will require power, and power always comes at a premium in implanted medical devices. For example, the battery packs in current DBS systems last for about 10 years, and getting the same kind of battery life from a dynamic system will require a great deal of upfront work to develop low-power embedded microprocessors.
Another research track will involve creating algorithms to properly interpret the incoming neural signals from the brain. Kemere's research group will rely heavily on experiments with rats to create, test and refine systems that can correctly interpret incoming neural signals and respond accordingly.
"We think we can optimize DBS stimulation and maximize its therapeutic benefit if we can better understand how information flows in the cortical-basal ganglia circuits in healthy brains, how those flows are disrupted by Parkinson's disease and how DBS can alter those flows," Kemere said.














