Scientists train immune system to spot and destroy cure-defying mutant HIV
Luring dormant HIV out of hiding and destroying its last cure-defying holdouts has become the holy grail of HIV eradication, but several recent attempts to do so have failed. Now the findings of a Johns Hopkins-led study reveal why that is and offer a strategy that could form a blueprint for a therapeutic vaccine to eradicate lingering virus from the body.
The findings, published online Jan. 7 in the journal Nature, show HIV eradication efforts have been stymied by the virus' ability to mutate beyond recognition, rendering it impervious to immune system destruction even when lured out of hiding. Going a step further, the scientific team successfully trained the immune system to recognize, attack and subdue such mutant HIV once coaxed out of its dormancy.
In a description of their "proof of principle" research, the team says they tamed mutant HIV by training a class of immune sentinel cells known as killer T cells to spot and eliminate HIV-infected cells capable of evading immune surveillance and impervious to immune system destruction.
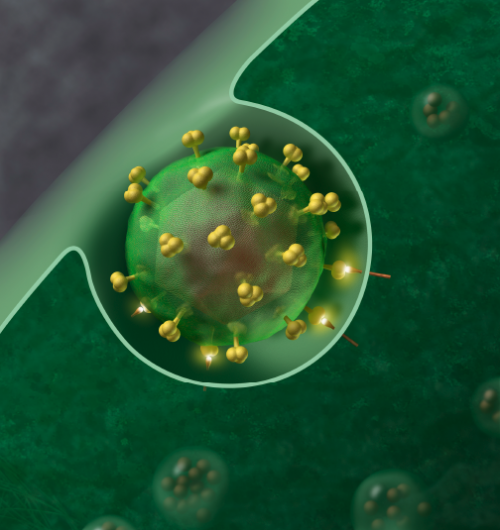
The strategy addresses one of HIV's most challenging behaviors—its ability to hijack a class of immune cells known as memory CD4+ T cells, where it goes into hiding soon after infection, lying quietly under the immune system's radar and unreachable by antiviral drugs. The killing of those last infected cells has become the focus of numerous recent efforts to lure the virus out of dormancy and finish it off permanently. However, the new findings show much of the latent virus is not merely out of reach, but also genetically altered to evade recognition by the immune system even once latency is reversed.
"Our results suggest that luring HIV out of hiding is winning only half the battle," says senior investigator Robert Siliciano, M.D., Ph.D., professor of medicine, molecular biology and genetics at the Johns Hopkins University School of Medicine. "We found that these pools of dormant virus carry mutations that render HIV invisible to the very immune cells capable of disarming it, so even when the virus comes out of hiding, it continues to evade immune detection."
Using a technique known as deep sequencing to reveal HIV's genetic features down to a single infected cell, scientists analyzed blood samples from 25 HIV-infected patients, 10 of whom had started therapy early—within three months of infection—while the rest had begun treatment after the three-month mark, when HIV infection enters its chronic stage.
Strikingly, the researchers report, they discovered that patients who began antiviral therapy within a few weeks or months of infection harbored largely non-altered HIV. Those who had started treatment later had viral reservoirs composed almost entirely of HIV that carried so-called escape mutations, which occur when key sections of the viral protein shape-shift beyond recognition. All viruses and bacteria carry such key protein identifiers. Intact, these identifiers are spotted by the immune system as "foreign," triggering an immune attack. However, soon after infection HIV quickly alters these "marker" regions, making them unrecognizable to the immune system. In the study, people who started therapy early appeared to have halted the mutation process in its tracks, freezing the virus more or less in its original state, the researchers found. By contrast, more than 98 percent of the virus in the latent reservoirs of late-treated patients was broadly altered. The good news, Siliciano and his colleagues report, is that each HIV-infected cell retains a tiny portion of its original viral protein intact—a feature the researchers exploited to test a possible solution to the "recognition" problem.
"We hypothesized that if these killer T cells were somehow nudged to spot the tiny segments of unaltered virus, they would kill the entire HIV-infected cell," says Kai Deng, Ph.D., lead author of the study and a postdoctoral research fellow at the Johns Hopkins University School of Medicine.
Just like unmasking a tiny portion of a camouflaged target allows a sniper to suddenly discern the hidden mark, researchers exposed killer T cells to the unaltered portions of the viral protein.
To do so, scientists first isolated killer T cells from patients and mixed them either with mutant forms of HIV or with a cocktail that contained both mutated and non-mutated lab-made chunks of HIV protein. After a few days, each group of killer T cells was exposed to cells infected with HIV obtained from patients carrying escape mutations. Killer T cells primed with the mixture of mutated and nonmutated HIV mounted a vigorous response against the patients' HIV-infected cells, killing 61 percent of them. By contrast, killer T cells primed only with mutant HIV showed a weak response and low kill rate, destroying only 23 percent of HIV-infected cells.
"It's as if the immune system had lost its ability to spot and destroy the virus, but priming killer T cells that recognize a different, nonmutated portion of HIV's protein reawakened that natural killer instinct," Siliciano says.
To see whether the primed killer T cells could perform outside the lab dish, the investigators injected them in a handful of so-called humanized mice, animals engineered to be physiologically closer to humans than standard lab mice. Each mouse received bone marrow from an HIV-infected patient, giving rise to a humanized immune system, and each mouse was then infected with HIV derived from the corresponding patient whose immune system the animal now harbored. All animals developed full-blown HIV infections. When investigators injected mice with patient-derived killer T cells primed solely by mutated viral proteins, the animals succumbed to the infection. In contrast, mice injected with retrained killer T cells—those primed with a mixture of mutant and nonmutant HIV—were able to control the infection and experienced a sharp thousand-fold drop in the amount of circulating virus. Some of the animals treated that way suppressed HIV below detectable levels.
"Our results shows that any curative strategy designed to eradicate HIV infection would need to include the use of killer T cells primed to recognize nonmutant forms of HIV," Deng says.
More information: K Deng et al. Broad CTL response is required to clear latent HIV-1 due to dominance of escape mutations. Nature DOI: 10.1038/nature14053 (2015).

















