HIV/AIDS drugs interfere with brain's 'insulation,' study shows
Antiretroviral therapies, or ART, have enabled people with HIV and AIDS to live much longer lives, transforming what was considered a death sentence into a chronic condition. Yet concerns for these patients remain. Up to half of people with HIV on these drug regimens have some sort of cognitive impairment, such as memory loss or problems with executive functioning, despite the virus being almost undetectable in their bodies.
In a new study, researchers from the University of Pennsylvania and The Children's Hospital of Philadelphia teamed up to investigate the underlying reasons for these impairments. They found that commonly used antiretroviral medications disrupted the function of oligodendrocytes, crucial brain cells that manufacture myelin, the fatty material that serves to insulate neurons, helping them transmit signals in the brain fast and efficiently.
This disruption, the researchers said, may be responsible for some of the cognitive problems that HIV patients experience, and point to a need for rethinking how HIV drugs are designed and prescribed, particularly for children on ART, in whom myelin is still forming at high rates.
"Pharmaceutical companies have done an amazing job developing drugs to make HIV patients live longer, but we're not done," said Kelly L. Jordan-Sciutto, professor and chair of Penn's School of Dental Medicine's Department of Pathology, who co-led the research with Judith B. Grinspan, a research scientist at CHOP and a professor of neurology at Penn's Perelman School of Medicine. "The message we want to get out there is that we want to make these patients' lives better while they are on ART."
The research was published this month in the Journal of Neuropathology and Experimental Neurology.
Jordan-Sciutto struck up a collaboration with Grinspan after hearing her describing her research on oligodendrocytes. Jordan-Sciutto had previously examined the effects of ART on neurons and astrocytes. Given the fact that people on ART had been found to have reduced white matter in their brains, it made sense to investigate how oligodendrocytes would be affected, since those cells produce the lipid-filled myelin that gives white matter its characteristic color.
Myelin production is concentrated in the first two years of life, and continues throughout childhood.
"Over the first two years of life you go from having hardly any control over your body to being able to control your limbs and walk," said Grinspan. "A lot of that is on account of myelination."
But even in adults, oligodendrocytes act to ensure myelin is properly maintained.
"If myelin is destroyed, nervous impulses will no longer travel smoothly along neurons and the now bare nerve process will also start to fall apart," Grinspan said.
To see if ART could affect myelin production, the researchers decided to look at how oligodendrocytes responded to the drugs. They chose to examine three drugs that were at one time part of the most commonly recommended drug combinations prescribed to HIV patients: protease inhibitors Ritonavir and Lopinavir as well as nucleoside reverse transcriptase inhibitor Zidovudine, commonly known as AZT.
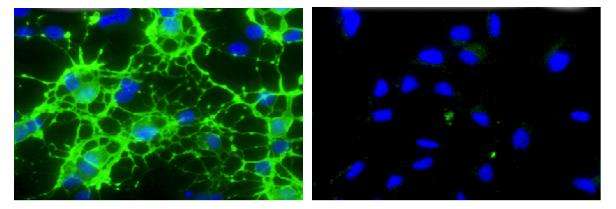
They first exposed mouse oligodendrocyte precursor cells to the three drugs at doses comparable to the concentration that would be found in plasma in an HIV patient under treatment. They found that Ritonavir and Lopinavir treatment reduced the cells' ability to mature and properly make myelin in a dose-dependent manner. AZT had no effect.
When they washed out the drugs from the cells, the effect was reversed, and oligodendrocytes were able to mature and make myelin once again.
"That told us that the drugs weren't simply killing the cells," Grinspan said. "They were creating some kind of defect that could be reversed."
Next the researchers administered Ritonavir to adult mice, selecting it because of its wide global use. After two weeks of treatment, they assessed the effect on myelin in the animals' frontal cortex and found that treated animals had significantly reduced levels of certain components of mature myelin.
Finally, the team used human brain tissue from autopsies of a cohort of HIV-infected patients provided by collaborator Benjamin B. Gelman at the University of Texas Medical Branch, to evaluate the effects of ART on myelin. They were able to sort the samples into categories based on age, whether the sample was from someone who received ART or was untreated, and whether someone had been diagnosed with a neurocognitive disorder.
They evaluated a sample of prefrontal cortex from each individual, looking for differences in myelin protein levels. When they compared the HIV-positive group to a control group of HIV-negative individuals they found no significant difference in myelin protein levels. When they specifically examined individuals who had a diagnosis of an HIV-associated neurocognitive disorder and were also on ART, they found a significant decrease in levels of the most critical myelin protein, myelin basic protein, or MBP, compared to both HIV-positive and HIV-negative groups.
The researchers have yet to determine a mechanism by which these myelin protein levels are altered with ART, but are investigating a number of avenues. They are also evaluating how different HIV medications can affect oligodendrocytes and myelin formation, as the recommended drug cocktails frequently change.
The implications of these findings may be particularly important for pediatric patients, some of whom may have been on ART from birth. Since it's known that ART treatments are associated with an increased risk of neurocognitive disorders such as autism, schizophrenia, manic depression and ADHD, the researchers stress that a revised look at treatments for pediatric patients may be warranted, or an additional therapy to prevent the white matter loss in both adults and children could be developed to go hand in hand with the ART.
Understanding the mechanisms of the drug effects on oligodendrocytes could also shed light on the function of oligodendrocytes in other conditions, such as multiple sclerosis, which is characterized by a loss of myelin in the brain.
More information: Brigid K. Jensen et al. Altered Oligodendrocyte Maturation and Myelin Maintenance, Journal of Neuropathology & Experimental Neurology (2015). DOI: 10.1097/NEN.0000000000000255

















