Genetically engineered immune cell therapy found to boost survival in mice with brain tumors
Nagoya University-led research team shows in mice the potential of a special immune cell that targets a key protein in tumor growth that helps stop brain cancer.
For decades most cancers have been treated with a core standard of treatments that include surgery, radiation, and chemotherapy. Now, immunotherapy—a type of treatment that harnesses the patient's immune system to combat the disease—represents the future of cancer treatment, with its efficacy being demonstrated in even the most aggressive types of cancer.
Brain cancer comes in many forms, ranging from more easily treatable benign forms that may trigger gradual loss of brain functions, to malignant forms that can in many cases prove fatal. While there have been improvements in the current standard treatments, patients with glioblastoma (GBM), the most common and aggressive form of brain tumor, still suffer from a median survival rate of only 14.6 months and 5-year overall survival rates of less than 10%. There is therefore pressing need for novel therapies that improve the outcomes.
Researchers at Nagoya University have been studying the therapeutic effect of T cells, vital disease-fighting components in our body's immune system, for fighting cancer.
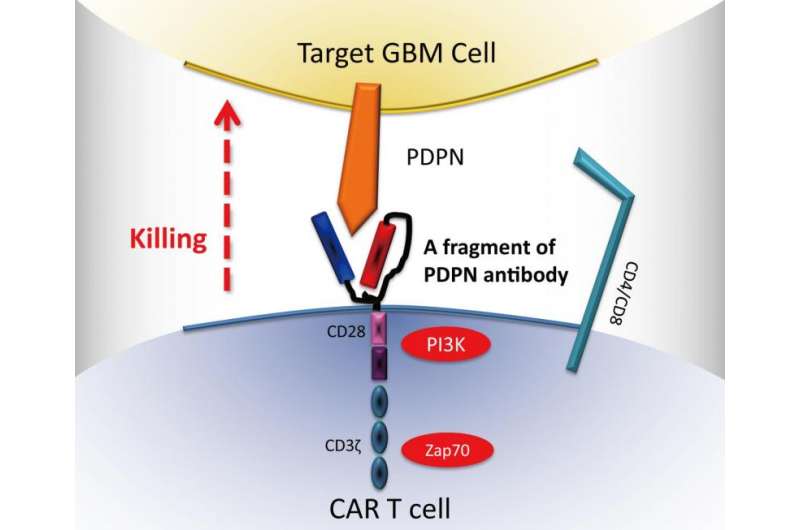
"Immunotherapy has emerged in recent years as a promising strategy for treatment of GBM," says Atsushi Natsume, corresponding author of the study and a member of the Nagoya University School of Medicine's Department of Neurosurgery. "We have successfully engineered T cells that produce special receptors on their surface, called chimeric antigen receptors (CARs), which allow the T cells to recognize specific proteins (antigens) expressed in GBM. We designed chimeric antigen receptor (CAR) T cells that specifically target podoplanin (PDPN), a key protein for the progression of solid tumors, including GBM."
The research team found that injection of CAR T cells into 79 immunodeficient mice arrested the growth of GBM in 60% of them. Furthermore, the T cells can recognize PDPN on the tumor surface even with the absence of the body's own immune recognition system, which is usually compromised in cancer.
"Considering that PDPN is associated with poor prognosis in GBM, CAR T-cell therapy that targets this protein is promising for treatment of patients with relapsed or resistant tumors following first-line chemotherapy," says Toshihiko Wakabayashi, a coauthor and the chair of Department of Neurosurgery Nagoya University School of Medicine. "There are certainly challenges to overcome for clinical application of this kind of immunotherapy, but the newly published data are an important milestone in immunotherapy targeting solid tumors that have eluded other treatments."
More information: S. Shiina et al. CAR T Cells Targeting Podoplanin Reduce Orthotopic Glioblastomas in Mouse Brains, Cancer Immunology Research (2016). DOI: 10.1158/2326-6066.CIR-15-0060
















