Researchers create a promising new treatment for the deadliest form of brain cancer
UCLA scientists have developed a potentially promising new combination therapy for glioblastoma, the most common and deadliest form of brain cancer.
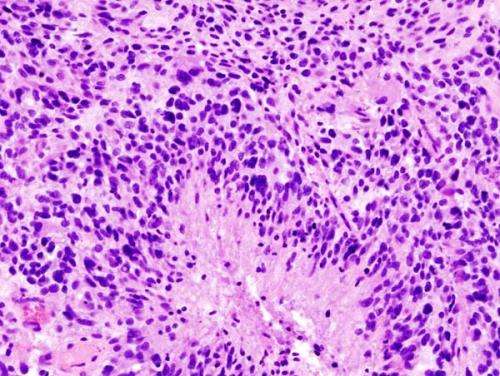
Glioblastoma, also known as grade IV glioma, is an aggressive primary brain tumor in humans. Approximately 23,000 people in the U.S. are diagnosed with glioblastoma every year. Patients usually receive surgery, chemotherapy and radiation, but these treatments are not very effective as an estimated 50 percent of GBM patients die within one year, and 90 percent die within three years.
A study led by Dr. Robert Prins and Dr. Linda Liau, both members of the UCLA Jonsson Comprehensive Cancer Center, looked at the impact of a combined treatment using a chemotherapy drug called decitabine and genetically modified immune cells. It is a continuation of previous research, published in 2011, that focused on the effect of decitabine on glioblastoma human cell cultures.
In the new research, Prins and Liau used a technique called engineered adoptive T cell transfer, which involves extracting and growing immune cells outside of the body, then reprogramming them with the gene for a T cell receptor targeting New York esophageal squamous carcinoma, or NY-ESO-1. They are then injected back into mice with glioblastoma tumors to produce an immune response that targets the brain cancer.
Glioblastoma cells do not naturally produce NY-ESO-1, so the researchers administered decitabine prior to injecting the reprogrammed T cells in order to cause the tumor cells to express the NY-ESO-1 target.
"The lymphocytes will seek out and find the glioblastoma cells in the brain," said Prins, UCLA associate professor in the departments of neurosurgery and molecular and medical pharmacology. "They can cross different fiber tracts in the brain to reach tumor cells that have migrated away from the main tumor mass. These factors are important in the treatment of invasive tumors, such as glioblastoma. While surgery to remove the main tumor mass can be done, it is not possible to then locate the tumor cells that get away and this ultimately leads to a nearly universal tumor regrowth."
This new method was about 50 percent effective at curing glioblastoma in the study.
"Brain cancer cells are very good at evading the host immune system, because they do not express specific targets that can be recognized by immune cells," said Liau, UCLA professor and vice chair of neurosurgery.
"By treating glioblastoma cells with decitabine, we found that we can unmask targets on the tumor cell that can be recognized by killer T cells. Once these targets are uncovered, we can then administer T cells that are genetically programmed to attack tumor cells with the new targets."
The next stage of Prins' and Liau's research will verify these findings in other brain tumor models.
This research will be published today in the journal Neuro-Oncology.



















