GI problems in autism may originate in genes, study suggests
Researchers at Columbia University Medical Center (CUMC) have found evidence in mice that, for some types of autism, gastrointestinal difficulties may originate from the same genetic changes that lead to the behavioral and social characteristics of the condition. The study was published in the Journal of Clinical Investigation.
Children with autism spectrum disorder are four times more likely to suffer from gastrointestinal problems than other children. These GI troubles are often blamed on the tendency of kids with autism to limit their diets to a few favored food items.
"Gastrointestinal issues have been recognized as a common occurrence in people with autism since the condition was first described in the 1940s, but there was no indication that they were directly related," says the study's lead author, Kara Gross Margolis, MD, associate professor of pediatrics at Columbia.
Recent research by Jeremy Veenstra-VanderWeele, MD, the Mortimer D. Sackler, MD Associate Professor of Psychiatry at Columbia, and Randy Blakely, PhD, professor of psychiatry at Vanderbilt University School of Medicine, had linked some cases of autism to genetic mutations that inhibit serotonin activity. Serotonin is a chemical that transmits signals from one neuron to another in the brain. The brain, however, contains only 5 percent of the body's serotonin; most of the rest is at work in the GI system. Genetic mutations that affect serotonin's activity will thus have ramifications in the gut as well as in the brain.
"Because serotonin plays an important role in the gastrointestinal system as well as the brain, we wanted to see if there was a direct relationship between these genes and GI development and function," says Dr. Margolis, who conducted the study with Michael Gershon, MD, professor of pathology & cell biology at Columbia and a leader in the field of neurogastroenterology.
The researchers investigated gastrointestinal development in a mouse model, created by collaborators at Vanderbilt, that carries a mutation found in some patients with autism. The mutation decreases serotonin activity by increasing the activity of the serotonin reuptake transporter (SERT), which pulls serotonin back into the neuron after it is released for neurotransmission.
Previously, the Vanderbilt researchers had shown that mice with the SERT mutation displayed behaviors that are strikingly similar to those seen in children with autism. In particular, the mice vocalized less, engaged in repetitive behaviors, and avoided contact with other mice.
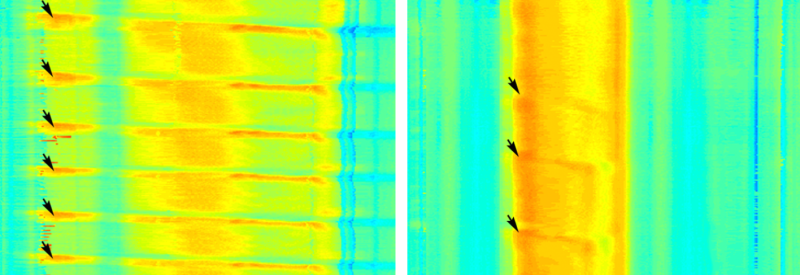
In the new study, Drs. Margolis and Gershon discovered that these mice have fewer neurons than normally found in the gut, a poorly maintained gut lining, and slower movement of gut contents. The changes were present in young mice and persisted through adulthood.
"Basically, the gut goes slower and the mice were constipated, which is a common complaint in kids with autism," Dr. Gershon says.
"Our study is one of the first to suggest that GI and neurological aspects of autism, in some cases, may stem from a shared underlying abnormality," says Dr. Margolis. "This provides scientific credibility to the idea that gastrointestinal problems may be an innate feature of autism, at least for some patients."
The study also found that the gastrointestinal changes in mice caused by the SERT mutation could be prevented if during pregnancy their mothers were given prucalopride, a drug that mimics the ability of serotonin to stimulate nerve cell development. "We see that we can prevent gastrointestinal changes in mice with the SERT mutation, but we still need to learn if we can reverse these changes once they appear," Dr. Margolis says.
Regardless of the root of the GI distress in patients, Dr. Margolis says families and physicians should recognize that gastrointestinal problems are common in children with autism. "The difficulty is that these kids present in a different way. Often, they're not verbal or they have sensory issues so they can't pinpoint where the pain is coming from," she says. "So it's important that when these patients present with distress or behavioral problems, a gastrointestinal source is considered."
Since low serotonin activity caused deficient development of gastrointestinal neurons, slow motility, and inadequate maintenance of the gastrointestinal mucosa, the researchers wanted to determine if high serotonin activity during development would increase generation of nerve cells, speed motility, and enhance mucosal maintenance.
The researchers increased serotonin activity in developing mouse pups by giving their mothers SSRI antidepressants (e.g., Prozac), which raise serotonin levels by inhibiting SERT, or by knocking out the SERT gene (SERTKO).
As expected, the pups had changes to their gastrointestinal systems that were the opposite of those found in the autism model mice. Whereas the autism model mice had too few gastrointestinal neurons and a slow-moving gut, the SSRI and SERTKO pups had too many neurons and a fast-moving gut. And while the intestinal lining of the autism model mice was too thin, the lining in the SSRI and SERTKO mice was too thick.
Only one study has looked at gastrointestinal disorders among children of women who take SSRIs during pregnancy. This study found that such children are 10 times more likely to have a gastrointestinal disorder than children from the general population.
"We're not advising anyone to stop taking SSRIs. Depression is not trivial in pregnancy and there are a lot of things to consider," Dr. Margolis says. "As physicians, we want to make people aware of all the side effects of the drugs they take, so they can make better-informed decisions."
More information: Kara Gross Margolis et al, Serotonin transporter variant drives preventable gastrointestinal abnormalities in development and function, Journal of Clinical Investigation (2016). DOI: 10.1172/JCI84877

















