A novel protein regulates cancer immunity and could offer a therapeutic target
In an article published online ahead of print on March 13, 2017 by the Journal of Clinical Investigation, Medical University of South Carolina (MUSC) investigators report preclinical research showing that moesin, a membrane-domain organizing protein, controls regulatory T cell (Treg) function as well as the abundance and stability of transforming growth factor-beta (TGF-beta) receptors on the surface of cells, providing a potential therapeutic target for cancer immunotherapy.
Their findings show that TGF-beta acts at the protein level to generate Tregs in the tumor microenvironment. Although the human immune system is capable of eradicating cancer, Tregs dampen the immune response and protect cancer cells against tumor-killing (i.e., cytotoxic) T cells. The MUSC study is the first to show that eliminating moesin reduces TGF-beta receptor expression and subsequent Treg generation to restore anti-tumor immunity.
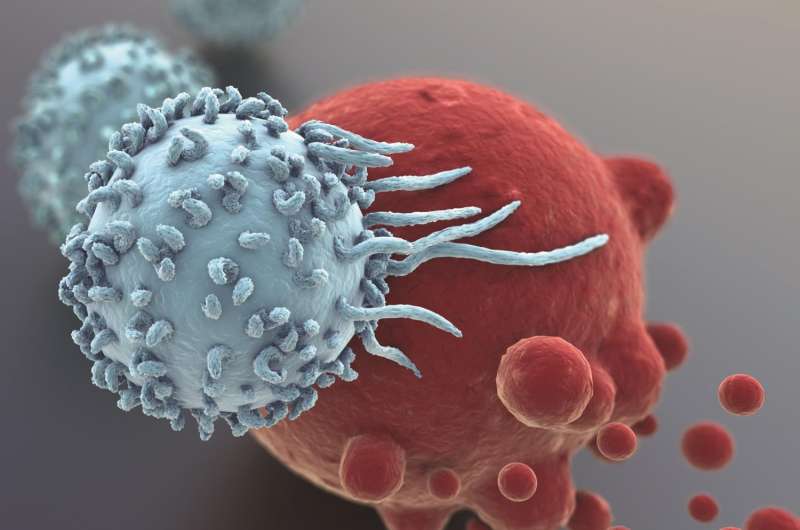
T cells, a subtype of white blood cells, can effectively attack and kill tumor cells when activated by the protein TGF-beta. However, the immune system has a sophisticated network of checks and balances to ensure that the body does not produce so many of these cytotoxic T cells that it harms its own cells and tissues. When the immune reaction is complete, TGF-beta signals naive T cells to become Tregs that suppress and degrade the activated, inflammatory T cells, ensuring that they do not overproduce the immune factors that can lead to autoimmune disease.
Cancer cells have learned to hijack this system of checks and balances to hide from the tumor-killing T cells. Many cancers produce TGF-beta that binds the receptors on the tumor-killing helper T cells so they can't be recruited to fight the tumor. The T cells convert instead to Tregs, which suppress the immune response against the cancer.
Inhibiting moesin could help prevent conversion of naïve T cells into Tregs, thereby restoring the anti-tumor immune response.
"Because moesin supports greater Treg production, we could design moesin inhibitors to halt or slow active TGF-beta signaling and slow down Treg conversion so that anti-tumor T cells can have a chance to see the cancer and eradicate it," explains Zihai Li, M.D., Ph.D., chair of the Department of Microbiology and Immunology at MUSC and senior author on the paper.
Earlier studies by Philip Howe, Ph.D., chair of MUSC's Department of Biochemistry and Molecular Biology and a co-author on the paper, demonstrated that many TGF-beta-mediated epithelial mesenchymal transition genes, including moesin, were repressed by an RNA-binding protein in healthy epithelial cells and that moesin expression could be restored through TGF-beta stimulation.
This ability of TGF-beta to dramatically increase moesin expression led the team to investigate moesin's role in Treg generation. Jointly with other colleagues at MUSC, the team compared the abilities of helper T cells with and without moesin to become iTregs. They found that moesin promotes Treg generation by interacting with a TGF-beta receptor (TβR-II) to make it more available, thereby enhancing TGF-beta signaling. Conversely, TGF-beta signaling was reduced in the absence of moesin, impairing the development and function of Tregs.
Perhaps the most compelling results were provided by studies involving adoptive T cell therapy in a mouse model of melanoma. In adoptive T cell therapy, tumor-killing T cells are "harvested" from a human or animal with cancer and amplified or otherwise "supercharged" before being reinfused into the donor. Although these reinfused cells can be very effective at killing tumors, they do not always survive long-term, setting the stage for recurrence.
The MUSC research team showed that these reinfused anti-cancer CD8+ T cells not only underwent rapid activation and expansion in mice lacking moesin, but that they also survived longer, reducing the likelihood of recurrence. Indeed, after adoptive T cell transfer, all of the mice having moesin relapsed while most of the mice lacking moesin were cured.
"When the mice lacking moesin had no recurrence, this was really exciting. We were not only deleting moesin but, when we gave T cells to the active tumors, those T cells could control the cancer for a very long time," explains Ephraim Ansa-Addo, Ph.D., a postdoctoral fellow in the Department of Microbiology and Immunology and lead author on the article.
These findings suggest that moesin could be a therapeutic target in developing new treatments for cancer and Treg-related immune disorders. Chemical modulators of moesin could control the function of T cells by inhibiting moesin in cancers or inducing it to treat autoimmune diseases. Moesin modulators could also be combined with current immunotherapy regimens.
"These findings are very interesting for the field and provide a lot of directions for further research into alternative therapies," says Li.
More information: Ephraim A. Ansa-Addo et al, Membrane-organizing protein moesin controls Treg differentiation and antitumor immunity via TGF-β signaling, Journal of Clinical Investigation (2017). DOI: 10.1172/JCI89281


















