New stenting tool could make heart procedures cheaper and less painful
A new tool for assessing the narrowing of the heart's arteries was found to be as effective as current methods and less painful for patients.
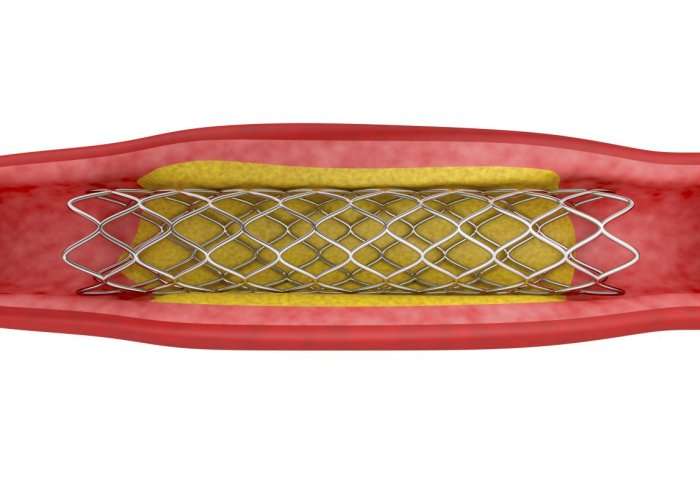
The tool is similar to current techniques in telling surgeons whether a patient needs a stent – a type of mesh tube used to hold open clogged arteries and increase blood flow. However, this new technique, known as instantaneous wave-free ratio (iFR), is much more pleasant for the patient, and could be cheaper and less time-consuming for healthcare providers.
Coronary stenosis occurs when various factors cause narrowing of the coronary arteries, which deliver oxygen-rich blood to the muscle of the heart.
When these blood vessels become blocked or are narrowed, this can affect how the heart functions, potentially leading to chest pain, heart attacks and heart failure.
Now, Dr Justin Davies and his team from the National Heart and Lung Institute at Imperial College London have developed iFR to measure the pressure loss caused by the narrowing in these important blood vessels without the need for drugs with sometimes unpleasant side effects. This novel technology was licensed to Volcano-Philips by Imperial Innovations, the College's technology transfer partner.
The technique received FDA approval in 2013 and is already used in 4,500 labs worldwide, but the latest study is the biggest yet to prove its effectiveness compared with the current most widely established technique.
"We have already seen iFR adopted into the latest 2017 appropriate use criteria (AUC) guidelines and expect this will lead to further changes in guidelines, which would have huge implications for cardiologists and their patients," said Dr Davies. "iFR technology is already used widely worldwide, and this is the study we've been waiting for to show that our technique is just as accurate as old ones, but far better for patients."
Deciding on stents
Measuring pressure in the coronary artery is important when deciding whether patients need to have a stent fitted – a procedure known as angioplasty. This helps to improve the blood supply to the heart muscle by widening the narrowed coronary arteries. However, before patients can undergo angioplasty, cardiologists must test the pressure of the artery to make sure it is narrow enough for a stent to be useful.
The first line technique in current guidelines, known as fractional flow reserve (FFR), requires using powerful drugs such as adenosine to open the blood vessels for easier measurement. However, it can cause severe crushing pain, low blood pressure and breathing difficulties, and adds more time and costs on to the procedure.
The latest study has shown that using the new technique (iFR) is just as accurate, causes less discomfort, is less time-consuming, and might be cheaper, than FFR. Click here for a live case demonstration of iFR, courtesy of Imperial College Healthcare NHS Trust.
Like FFR, iFR measures pressure using a thin wire in the coronary artery, but unlike FFR, it uses a mathematical algorithm to take measurements only when the heart is relaxed and the coronary blood flow is high, negating the need for adenosine.
In this study, the researchers enrolled 2,492 patients in 17 countries who suffered with chest pain or acute coronary syndrome (heart attack). They randomly assigned participants to undergo iFR or FFR, and either inserted a stent or not, depending on the measurements. Patients were followed up for 12 months after the procedure.
By measuring subsequent heart attack and mortality after FFR and iFR, the researchers were able to tell whether the type of technique used had any association with higher mortality or other outcomes.
Although there were no significant differences in rates of death or subsequent heart attack between the two techniques, patient experience was much improved with the iFR technique.
The researchers found that adverse events occurred in 31 per cent of FFR patients and three per cent of iFR patients overall.
FFR was also associated with a higher rate of shortness of breath (reported in one per cent of iFR patients and 20 per cent of FFR patients); chest pain (nearly two percent in iFR and seven per cent in FFR); heart rhythm disturbances (nearly zero per cent in iFR and nearly five per cent in FFR); abnormally low blood pressure (nearly zero per cent in iFR and one per cent in FFR); and serious adverse events, which included severe shortness of breath or disturbance of normal heart rhythm (nearly zero per cent in iFR and nearly one per cent in FFR).
They also found that iFR reduced the overall length of the procedure, from an average of 45 minutes for FFR to 40 minutes for iFR.
The results from this trial, known as DEFINE-FLAIR, are published in the New England Journal of Medicine, and are presented today at the American College of Cardiology's 66th Annual Scientific Session in Washington.
Lead author Dr Davies said: "As our technique eliminates the need for adenosine and reduces the length of the procedure, it could mean that iFR saves healthcare providers money. The study also provides a very good, real-world snapshot of the time it takes to actually get a patient in, do the physiological assessment, do the stenting if necessary, and finish."
Co-author of the study, Dr Sayan Sen, said: "'Cardiologists have been waiting for someone to prove that this new technique is just as effective as the current one."
"Many of our physician colleagues have been waiting for these results, and for them to be incorporated fully into the guidelines they use. DEFINE-FLAIR gives guideline makers the evidence they need to go ahead and suggest the technique that's better tolerated by patients, and more cost effective for the health service."
Next, Dr Davies and co-investigator Professor Javier Escaned will further analyse this data to fully compare the costs of iFR and FFR. They will also work to combine data from another study testing iFR outcomes, SWEDEHEART, with their own. The two groups of researchers will work together to conduct a follow-up analysis combining the data from the two studies in a meta-analysis of primary outcomes that will include approximately 4,500 patients.
More information: Justin E. Davies et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI, New England Journal of Medicine (2017). DOI: 10.1056/NEJMoa1700445
















