February 2, 2018 report
Team in China grows ears and attaches them to human patients
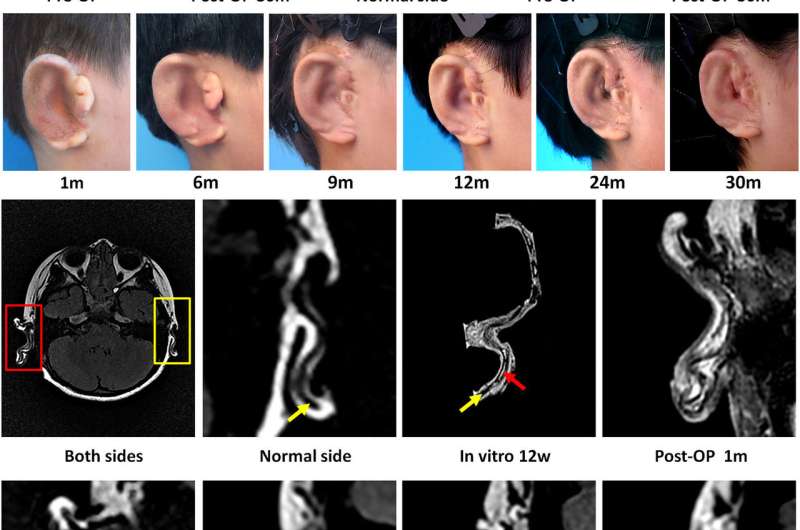
A team of researchers in China has, for the first time, created new ears for human patients by growing cartilage and implanting it. In their paper published on the open access site EBioMedicine, the group outlines how the ears were made, how they were attached and how well the ears are developing in the young patients.
All of the patients in the study were children (above age six, the point where ears stop growing) with a condition called microtia, in which one ear fails to develop normally or at all. Each volunteered for the study, which involved removing cartilage samples (chondrocytes) from the underdeveloped ear and then waiting three months for new ear cartilage to grow sufficiently for implantation. Cells taken from the cartilage were used to seed a scaffold built using a PCL mesh as an inner base, which was then wrapped with PGA fibers and then covered with PLA—all of which are biodegradable. The scaffold was housed inside a mold made using a 3-D model of each child's healthy ear. The mold allowed the cells on the scaffold to grow into the shape of normal ear cartilage.
After three months, the children had excess ear material surgically removed or altered—once fully prepared, the scaffold with its load of cells was implanted into the prepped ear, which was then covered with skin grafts. After that, the cartilage was allowed to mature on its own inside the child's ear over time. The researchers monitored each of the children for months, or even a couple of years, to see how the ears matured and to deal with any problems that arose. They report that for three of the five patients, the ears remained normally shaped—the other two had some slight shape abnormalities.
The researchers report that they will continue to monitor the patients for at least five more years, looking specifically for abnormal growth that could indicate tumors—implanted cultured cells have sometimes become cancerous in animal studies. Another concern is that the ears will become malformed over time because the cartilage is based on chondrocytes taken from the unhealthy ear.
More information: Guangdong Zhou et al. In Vitro Regeneration of Patient-specific Ear-shaped Cartilage and Its First Clinical Application for Auricular Reconstruction, EBioMedicine (2018). DOI: 10.1016/j.ebiom.2018.01.011
Abstract
Microtia is a congenital external ear malformation that can seriously influence the psychological and physiological well-being of affected children. The successful regeneration of human ear-shaped cartilage using a tissue engineering approach in a nude mouse represents a promising approach for auricular reconstruction. However, owing to technical issues in cell source, shape control, mechanical strength, biosafety, and long-term stability of the regenerated cartilage, human tissue engineered ear-shaped cartilage is yet to be applied clinically. Using expanded microtia chondrocytes, compound biodegradable scaffold, and in vitro culture technique, we engineered patient-specific ear-shaped cartilage in vitro. Moreover, the cartilage was used for auricle reconstruction of five microtia patients and achieved satisfactory aesthetical outcome with mature cartilage formation during 2.5 years follow-up in the first conducted case. Different surgical procedures were also employed to find the optimal approach for handling tissue engineered grafts. In conclusion, the results represent a significant breakthrough in clinical translation of tissue engineered human ear-shaped cartilage given the established in vitro engineering technique and suitable surgical procedure.
© 2018 Medical Xpress
















