Reducing unnecessary medication for hepatitis B patients
Not all chronic hepatitis B (HBV) patients require lifelong treatment; but the risks of blindly withdrawing treatment can be severe. However, there's little consensus on which patients can be safely discontinued from treatment, highlighting a clear need for a reliable biomarker of post-treatment HBV suppression. Working towards this goal, a team led by A*STAR and Duke-NUS researcher, Antonio Bertoletti, discovered that patients able to discontinue therapy without relapse share the trait of increased HBV-specific immune T cell response.
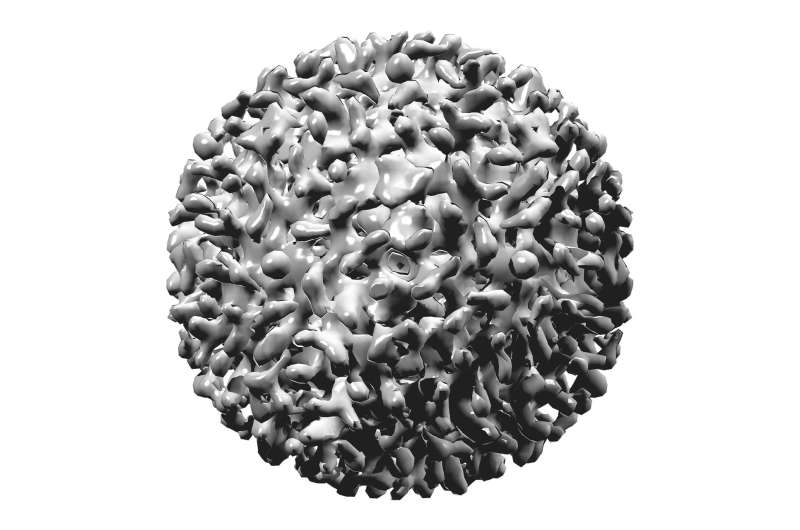
More than 400 million people suffer from chronic HBV infection. Unlike acute infection, which survivors can overcome and develop immunity to, chronic sufferers are prone to liver inflammation and are subsequently placed on medication indefinitely to suppress viral replication and minimize liver damage—a considerable financial burden and drug toxicity risk. But recent studies have indicated that the immune systems of some chronic HBV patients can control HBV replication and maintain liver health even after treatment ceases. Despite this, stopping treatment remains a dangerous stab in the dark: "In most patients, withdrawing therapy causes a strong rebound of the HBV replication, carrying a high risk of severe liver damage," says Bertoletti.
To identify predictive biomarkers that can help to select chronic HBV patients who can safely stop antiviral treatment, Bertoletti's team recruited 19 chronic HBV patients and observed them during therapy withdrawal for up to two years. They found that heightened levels of HBV-targeting T cells—especially CD8+ T cells expressing a protein called PD-1—were associated with patient health after medication was withdrawn. Bertoletti's team suggest that PD-1 may promote long-term CD8+ T cell survival and antiviral capabilities in chronic HBV patients.
The team verified their findings in a second cohort of 27 patients treated with a different antiviral therapy. The results confirmed that increased HBV-specific T cells are indicative of a patient's capacity to safely discontinue treatment, offering a biomarker with potential for the clinic.
Further work needs to be done before this discovery can benefit patients widely. Bertoletti's team, publishing their findings in the Journal of Clinical Investigation, note that the complex methodology required to analyze HBV-specific T cells requires specialized knowledge and skills not available in every lab. "We are now trying to develop a quick and easy method to measure HBV-T cells, and an assay that can be performed easily, even in hospitals," says Bertoletti.
More information: Laura Rivino et al. Hepatitis B virus–specific T cells associate with viral control upon nucleos(t)ide-analogue therapy discontinuation, Journal of Clinical Investigation (2018). DOI: 10.1172/JCI92812

















