Trust in science at root of vaccine acceptance
Results of a global research project, led by Eva Pressman, M.D., and Tim Dye, Ph.D., with the University of Rochester Medical Center (URMC), indicate that trust in science is the most powerful determinant of whether a person will decide to get a COVID vaccine.
The development of the COVID vaccines has been hailed a remarkable scientific achievement and there is broad consensus among government leaders, scientific experts, and the health care community that widespread vaccination is key to lowering the mortality and burden of the disease. And yet more than a year after the approval of the first COVID vaccine, a significant portion of the population—approximately 25 percent in the U.S.—eligible to receive the vaccine have chosen not to do so.
Understanding the underlying sources of vaccine hesitancy are an important public health priority, as the coronavirus pandemic continues to impact daily life. Pressman and Dye, both professors in the URMC Department of Obstetrics and Gynecology, led a team of researchers that analyzed data from online surveys conducted in the early stages of the pandemic in the spring of 2020. The results were recently published in the journal BMJ Open.
COVID vaccines were not available at the time, but were already under development. Participants were recruited via social media platforms such as Facebook and Instagram, and the surveys were translated into English, Spanish, French, and Italian. Responses were collected from more than 7,400 participants in 173 different countries.
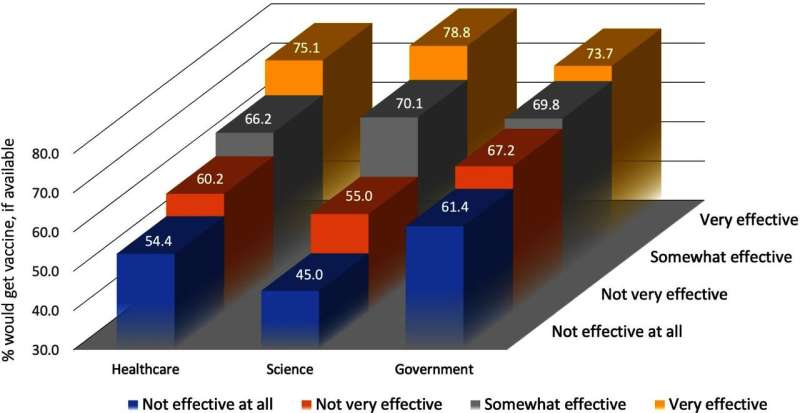
One of the key objectives was to understand the association between vaccine acceptance or hesitancy and trust in institutions—science, government, and health care—that would play key roles in convincing the public to get vaccinated. The study found that trust in science—namely the ability of biomedical research to produce a safe and effective vaccine—had the most impact on the decision to get vaccinated. They also found vaccine acceptance was higher in younger ages (under 32 years old) and those with more education. Further, people indicating they were unlikely to obtain a COVID vaccine were also less likely to socially distance or to stay home from school or work, and reported lower social support from friends, family, and significant others.
The science trust gap has many potential sources, according to the authors. Scientific literacy plays an important role. The conduct of science inherently takes time, can generate a range of findings, and studies often have limitations based on their scope and methodology, factors that make it vulnerable to conspiracy theories and misrepresentations. Science-informed policy is also vulnerable to politicization and in many communities there is a historic mistrust of science due to past abuses.
Overcoming resistance to COVID- 19 vaccination relies on enhancing communication to better explain science and policy options for disparate public audiences, according to the authors. "Clear and careful scientific communication is paramount in relaying support for scientific-based policies." The authors also recommend employing community-based and non-governmental organizations, such as the Red Cross, to help build public trust in COVID vaccines.
More information: Timothy D Dye et al, Science, healthcare system, and government effectiveness perception and COVID-19 vaccination acceptance and hesitancy in a global sample: an analytical cross-sectional analysis, BMJ Open (2021). DOI: 10.1136/bmjopen-2021-049716





















