This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Optimizing immunosuppression based on antibody testing does little to reduce kidney transplant failure rate, finds study
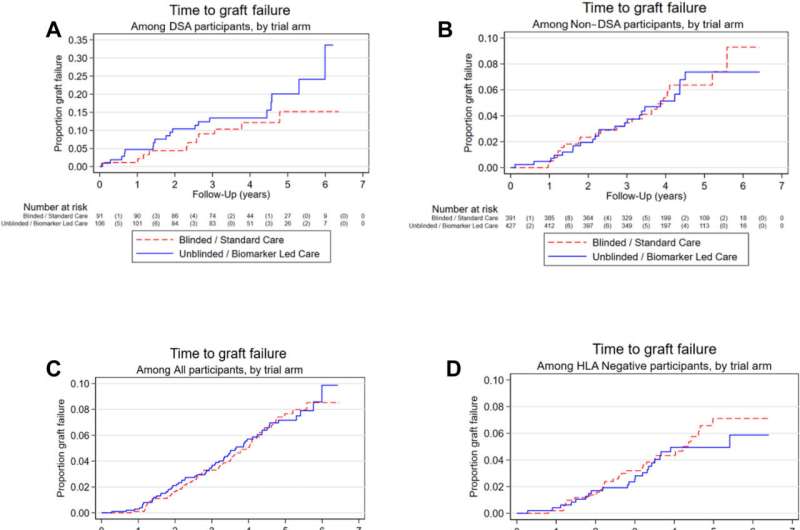
Treating patients who possess transplant rejecting antibodies, using best available combinations of oral drugs, does not have an impact on transplant failure rates but it does improve medication adherence and reduce rejection rates.
Kidney transplantation is the gold-standard treatment for kidney failure, yet thousands of kidney transplants fail each year because of the immune system attacking the transplanted organ. Finding antibodies against the transplant that are circulating the body can identify patients at risk of failure, sometimes years in advance.
The OuTSMART trial, led by King's and involving investigators from 13 UK transplant centers, recruited over 2000 transplant patients, split them into two groups randomly and screened them for circulating antibodies. Their findings, recently published in eClinicalMedicine, have the potential to impact clinical practice worldwide.
Patients in the intervention group were tested, told their antibody results and—if positive—they were encouraged to improve adherence to their immunosuppressive medicines. They were offered tailored treatment to a combination of the three best drugs available (tacrolimus, mycophenolate, and prednisolone) and presented with a regimen that was judged optimal for their individual needs.
In the control group, patients and doctors remained 'blinded' to their antibody test results and all treatment decisions were based on the pre-existing local standard of care. The trial confirmed that patients with antibodies were at higher risk of transplant failure but found no differences in failure rates between those who had the intervention compared to those treated by standard of care.
Transplant failure occurred despite the investigators being able to show increased medication adherence and a reduced rate of rejection in the intervention group. While transplant rejection and failure can be connected, transplant failure—causing the patient to go back to dialysis—is different to rejection and the two outcomes can occur independently of one another.
While the changes tested in the intervention group are currently recommended in guidelines issued by most transplant societies around the world, this study shows that the current standard of care produces similar results to the recommended antibody testing intervention. These findings are bound to have a significant impact on clinical practice.
"The problem we addressed in OuTSMART , that transplants do not last for the natural lifespan of most recipients, is one of the most important problems remaining in transplant medicine. The fact that we can deliver such a trial, despite the project taking over 10 years, is a real testament to the spirit of cooperation between UK transplant units and the willingness of transplant patients in the UK to help with research projects addressing important questions. Although this time we didn't find a way to prolong transplant survival, the unambiguous result will hopefully incentivize further research into new strategies to prevent transplant failure," says Professor Anthony Dorling, chief investigator and lead author.
More information: Dominic Stringer et al, Optimized immunosuppression to prevent graft failure in renal transplant recipients with HLA antibodies (OuTSMART): a randomised controlled trial, eClinicalMedicine (2023). DOI: 10.1016/j.eclinm.2022.101819




















